O'Neill, Derek, Condron, Ita, Kelleher, Cathy  ORCID: https://orcid.org/0000-0002-1754-0244, Lyons, Suzi, Mongan, Deirdre
ORCID: https://orcid.org/0000-0002-1754-0244, Lyons, Suzi, Mongan, Deirdre  ORCID: https://orcid.org/0000-0003-3616-4253 and Millar, Sean
ORCID: https://orcid.org/0000-0003-3616-4253 and Millar, Sean  ORCID: https://orcid.org/0000-0003-4453-8446
(2023)
Analysis of national drug and alcohol data by regional health area.
Drugnet Ireland,
Issue 84, Winter 2023, insert,
pp. 14-22.
ORCID: https://orcid.org/0000-0003-4453-8446
(2023)
Analysis of national drug and alcohol data by regional health area.
Drugnet Ireland,
Issue 84, Winter 2023, insert,
pp. 14-22.
| Preview | Title | Contact |
|---|---|---|
|
PDF (Drugnet Ireland 84, insert)
- Supplemental Material
661kB | |
|
PDF (Drugnet Ireland 84)
1MB |
This article presents the most recently available drug and alcohol data on treatment demand, general population prevalence, and opioid prevalence analysed by regional health area in Ireland.
1. Alcohol and drug treatment by regional health area
Background
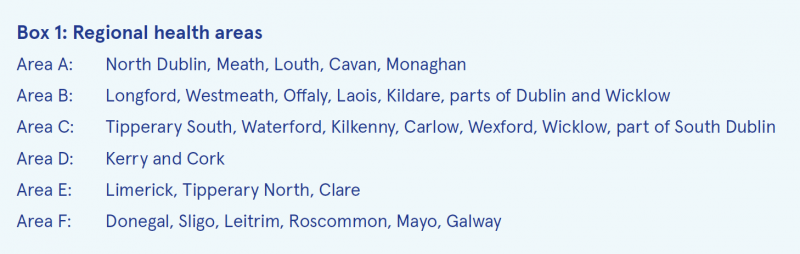
Sláintecare is the Irish Government’s 10-year programme for transforming how healthcare is delivered in Ireland.1 It aims to give equal access to services, with a vision of a universal health service, under the banner of Right Care, Right Place, Right Time. Part of this process is the creation of new healthcare areas that are based on population data, including on how people currently access services, in addition to being informed by a public consultation. In total, there are now six regional health areas (RHA) (see Box 1), encompassing 96 Community Health Networks (CHN).
Ensuring that the National Drug Treatment Reporting System (NDTRS) can provide data for the new Sláintecare areas will support the current Sláintecare reform programmes.2
- Programme 1: Improving Safe, Timely Access to Care and Promoting Health and Wellbeing is focused on integration, safety, prevention, shift of care to the right location, productivity, extra capacity, and achieving Sláintecare waiting time targets.
- Programme 2: Addressing Health Inequalities is focused on a journey towards universal healthcare.
Methods
The NDTRS is the national epidemiological surveillance database that records and reports on treated problem drug and alcohol use in Ireland. Established in 1990, the NDTRS is maintained by the National Health Information Systems (NHIS) of the Health Research Board (HRB) on behalf of the Department of Health. Treatment for problem alcohol and drug use in Ireland is provided by statutory and non-statutory services, including residential centres, community-based addiction services, general practices, and prison services. The NDTRS records cases of treatment, as there is currently no national system-wide unique identifier in the Irish health system. In any given year, individuals may appear more than once if treated in different centres or if they return to treatment in the same centre.
NDTRS data are recorded on LINK, an online reporting tool. LINK utilises Health Atlas Ireland to record geographical markers automatically as cases are entered. Through Health Atlas, the NDTRS currently records small area (SA), community healthcare organisation (CHO), local health office (LHO), electoral division (ED), county, and task force area (TFA). Using a mapping guide provided by the Central Statistics Office (CSO), and existing geographical markers in LINK, it was possible to derive RHA and CHN from the current and historical NDTRS data. NDTRS data were then analysed using RHA to describe the national treatment data based on where the client resided in the 30 days prior to treatment.
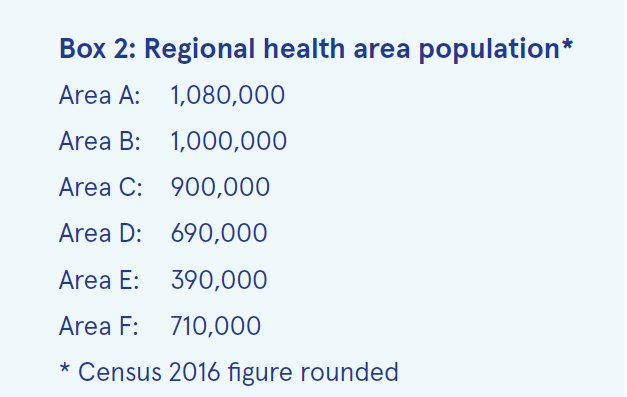
The population for each RHA varies, ranging from 390,000 (Area E) to 1,080,000 (Area A) (see Box 2). Rates of treatment cases per 100,000 population for both alcohol (see Table 4) and drugs (excluding alcohol) (see Table 5) as main problems were analysed using Census 2016 population data for each RHA.
Results
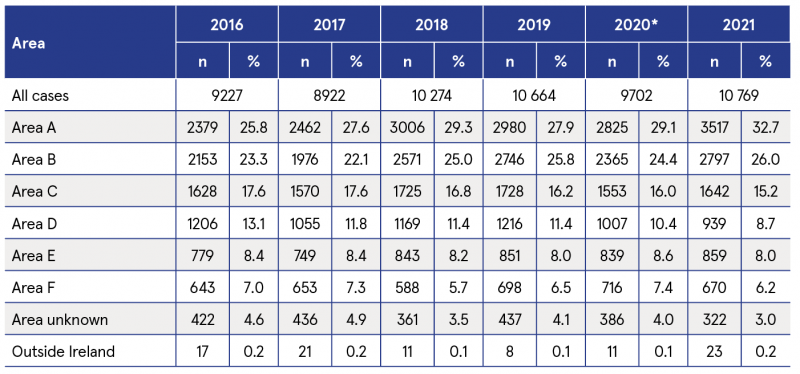
Between 2016 and 2021, Area A (North Dublin, Meath, Louth, Cavan, Monaghan) accounted for the highest proportion (24.9%) of treatment episodes (drugs and alcohol) nationally (see Table 1). The lowest proportion of episodes (7.8%), where RHA is known, occurred in Area E (Limerick, Tipperary North, Clare) (see Table 1). A small proportion of episodes (3.3%) could not be attributed to an RHA, either because the client address was not known (3.0%) or the client resided outside of Ireland (0.3%).
Over the period 2016–2021, Area C (Tipperary South, Waterford, Kilkenny, Carlow, Wexford, Wicklow, part of South Dublin) accounted for the highest proportion (21.6%) of cases reporting alcohol as a main problem nationally, followed by Area A (19.3%) (see Table 2). Area E had the lowest proportion of such cases (7.0%).
Table 1: Number of cases treated for drugs or alcohol as a main problem, by RHA and year, NDTRS 2016-2021
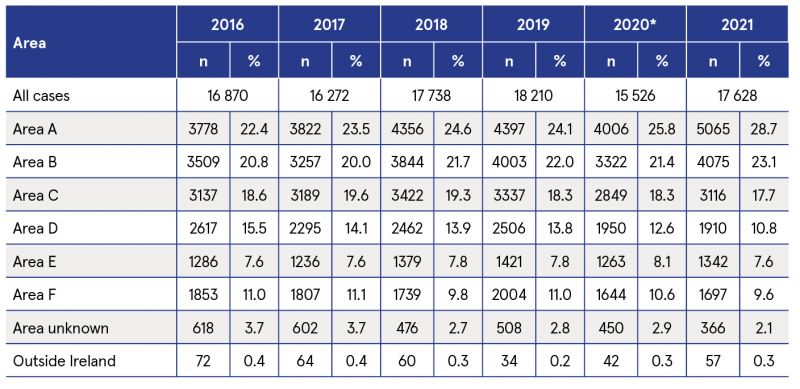
* Treatment figures impacted by the Covid-19 pandemic.
Table 2: Number of cases treated for alcohol as a main problem, by RHA and year, NDTRS 2016–2021
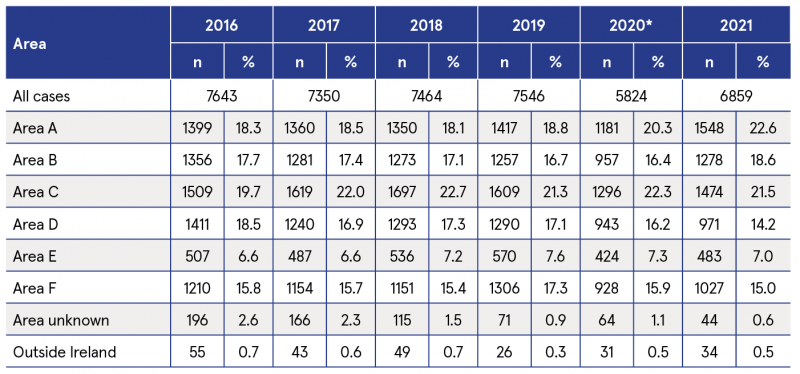
*Treatment figures impacted by the Covid-19 pandemic.
Over the period, Area A accounted for the highest proportion (28.8%) of cases of drug treatment (excluding alcohol), followed by Area B (Longford, Westmeath, Offaly, Laois, Kildare, parts of Dublin and Wicklow) (24.5%). Area F (Donegal, Sligo, Leitrim, Roscommon, Mayo, Galway) had the lowest proportion (6.7%) of drug treatment cases (see Table 3).
Table 3: Number of cases treated for drugs (excluding alcohol) as a main problem, by RHA and year, NDTRS 2016–2021
*Treatment figures impacted by the Covid-19 pandemic.
In 2021, the number of alcohol treatment cases per 100,000 population at RHA-level ranged from 123.8 (Area E) to 163.8 (Area C) (see Table 4). All areas experienced a substantial drop in treatment figures in 2020, due to the Covid-19 pandemic. In 2021, many of the areas had not yet returned to pre-pandemic numbers accessing treatment.
In 2021, the number of drug treatment (excluding alcohol) episodes per 100,000 population at RHA-level ranged from 94.4 (Area F) to 325.6 (Area A) (see Table 5). Treatment figures for 2020 were impacted by the Covid-19 pandemic in almost all areas. However, most areas had returned to pre-pandemic levels in 2021.
Table 4: Number of cases treated for alcohol as a main problem per 100,000 of RHA population, by RHA and year, NDTRS 2016–2021
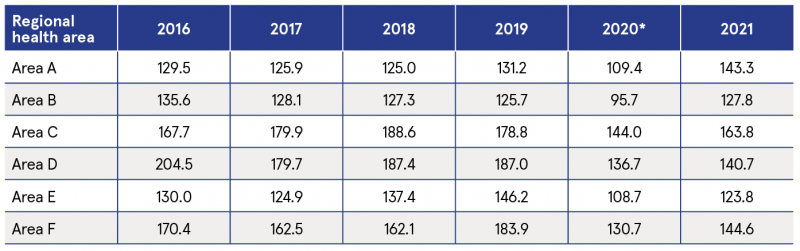
*Treatment figures impacted by the Covid-19 pandemic.
Table 5: Number of cases treated for drugs as a main problem per 100,000 of RHA population, by RHA and year, NDTRS 2016–2021
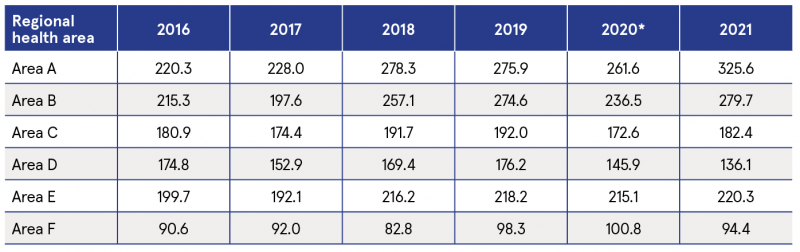
*Treatment figures impacted by the Covid-19 pandemic.
Discussion
NDTRS episode-based addiction treatment data for RHAs and CHNs can assist with developing a population-health approach for service planning and funding in addiction services, monitor access to addiction services by socially excluded groups, and inform any population-based resource allocation funding model.
The NDTRS has a coverage of over 70% of all applicable services, but this analysis did not take into account the impact of those services that do not participate in the NDTRS. At the higher RHA level, the impact is likely to be minimal, but at a CHN level the variation in participation could hinder efforts to understand addiction treatment service needs and potential inequalities in access. Greater cross-organisation communication between the HRB, funders and stakeholders, and services would assist in addressing this gap.3
2. Analysis of 2019–20 National Drug and Alcohol Survey by regional health area
Introduction
In 2018, the HRB commissioned IPSOS MRBI to conduct the fifth Irish National Drug and Alcohol Survey (NDAS). The 2019–20 NDAS followed best practice guidelines recommended by the European Monitoring Centre for Drugs and Drug Addiction. The questionnaire, based on the European Model Questionnaire, was administered in face-to-face interviews with respondents aged 15 years and older. A sample comprising all households throughout Ireland was randomly selected to participate. To facilitate comparisons between the 10 regional drug and alcohol task force (RDATF) areas, sampling was undertaken by RDATF area to enable the estimation of drug use prevalence in each area and to allow for monitoring of drug prevalence trends over time. Fieldwork began in February 2019 and was completed in March 2020. Of the household members contacted, 5,762 agreed to take part. The sample was weighted by sex, age, and region to ensure that it was representative of the general population. A more comprehensive description of the NDAS methodology is provided in the survey’s technical report.4
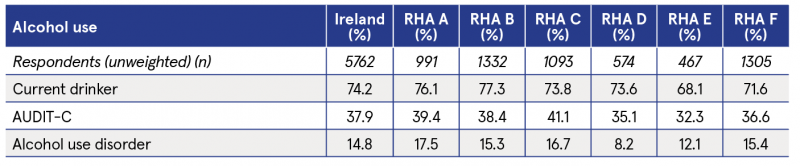
Alcohol use
Almost three-quarters (74.2%) of respondents were current drinkers (defined as those who had used alcohol in the last year). This ranged from 68.1% in Area E to 77.3% in Area B (see Table 6). Hazardous drinking was measured using the World Health Organization’s Alcohol Use Disorders Identification Test–Concise (AUDIT-C) screening tool. Among the whole sample, 37.9% met the criteria for hazardous drinking, which ranged from 32.3% in Area E to 41.1% in Area C. Alcohol use disorder (AUD) was measured using the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). There was considerable variation in the prevalence of AUD, from 8.2% in Area D (Kerry and Cork) to 17.5% in Area A. The overall prevalence of AUD in Ireland was 14.8%.
Table 6: Prevalence of current drinking, hazardous drinking, and alcohol use disorder, by RHA
Illegal drug use
In Ireland, 7.4% of adults reported use of any illegal drug in the previous year (see Table 7). Last-year prevalence of any illegal drug was lowest in Area E (6.1%) and highest in Area B (8.7%). There were differences in the types of drug use across RHA. In Area F, last-year prevalence of cannabis was relatively low (4.7% vs 5.9% nationally) and it also had the lowest prevalence of cocaine use (0.9% vs 1.9% nationally). However, it had the highest prevalence of ecstasy use (4.0% vs 2.2% nationally) and LSD use (2.8% vs 0.9% nationally).
Table 7: Prevalence of last-year drug use, by drug type and RHA
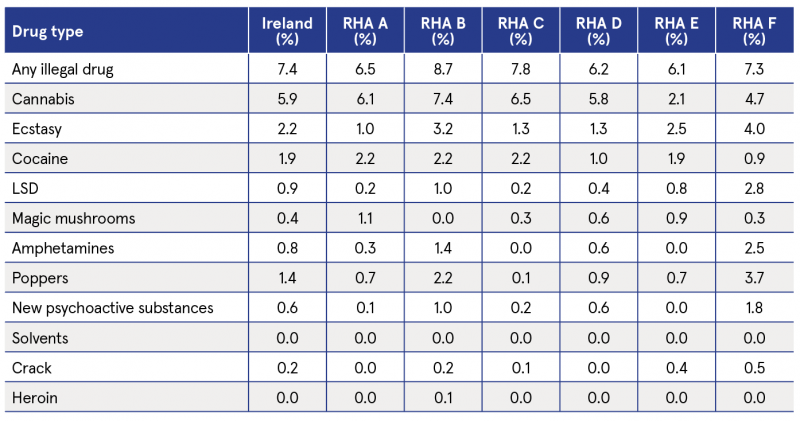
Table 8: Prevalence of last-year cannabis use disorder, by RHA
Last-year prevalence of cannabis use was 5.9% in Ireland, ranging from 2.1% in Area E to 7.4% in Area B. The prevalence of ecstasy use ranged from 1.0% in Area A to 4.0% in Area F. There was less variation in the prevalence of cocaine use; last-year prevalence was low in Area D and Area F (1.0% and 0.9%, respectively) and ranged from 1.9% to 2.2% in the four other RHA areas.
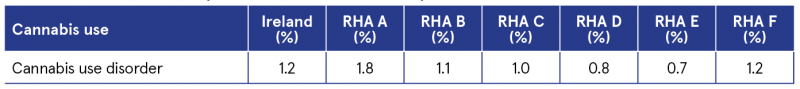
Cannabis use disorder (CUD) was defined as any cannabis abuse or dependence in the 12 months prior to the survey and was measured using an instrument called the Munich-Composite International Diagnostic Interview (M-CIDI). The last-year prevalence of CUD was 1.2% in Ireland and ranged from 0.7% in Area E to 1.8% in Area A (see Table 8).
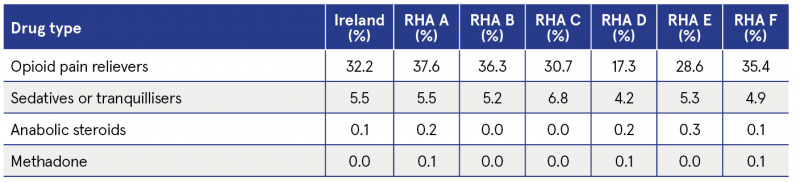
Use of prescribable drugs
Last-year prevalence of opioid pain relievers was 32.2% in Ireland, ranging from 17.3% in Area D to 37.6% in Area A. There was less variation in the prevalence of sedatives or tranquillisers; last-year prevalence nationally was 5.5%, ranging from 4.2% in Area D to 6.8% in Area C (see Table 9).
Table 9: Prevalence of last-year use of prescribable drugs, by drug type and RHA
Impact of drug use on local communities
Questions about the impact of drug use on local communities and drug-related intimidation were included in the 2019–20 NDAS for the first time. Three in 10 (30.5%) of respondents reported that there was a very big or fairly big problem with people using or dealing drugs in their local area (see Figure 1). People living in Area B were most likely to state that this was a big or fairly big problem (40.7%).
One in 10 respondents (9.9%) had either personal experience of drug-related intimidation or knew somebody who had been intimidated. People living in Area A (13.0%) and Area B (13.8%) were most likely to report an experience of drug-related intimidation (see Figure 2).
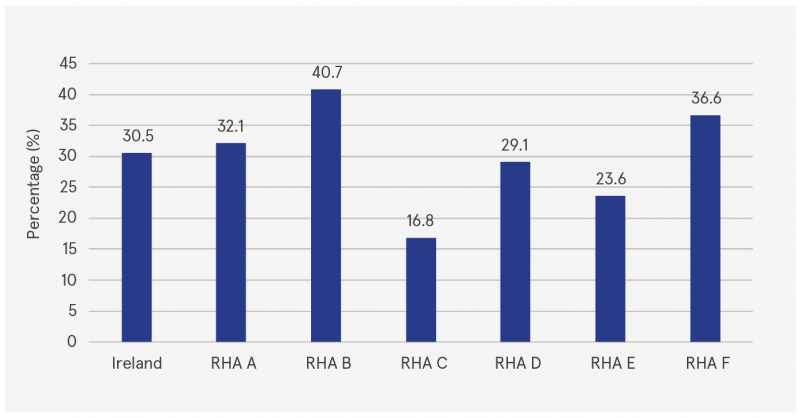
Figure 1: Proportion of respondents reporting that people using or dealing drugs was a very big or fairly big problem in their local area, by RHA
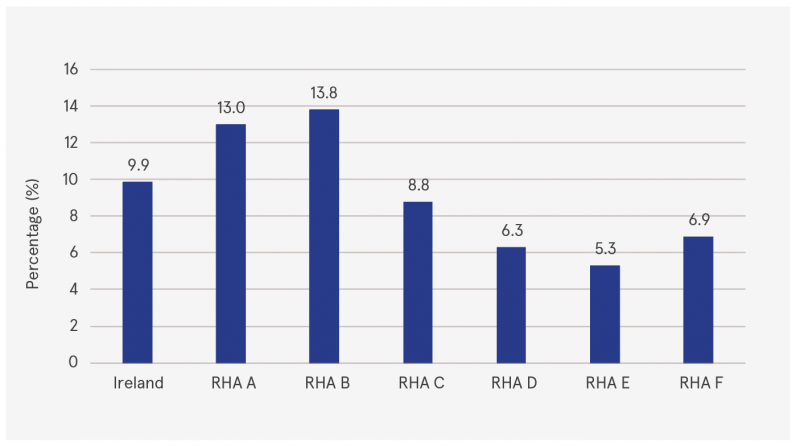
Figure 2: Proportion of respondents reporting experience of drug-related intimidation, by RHA
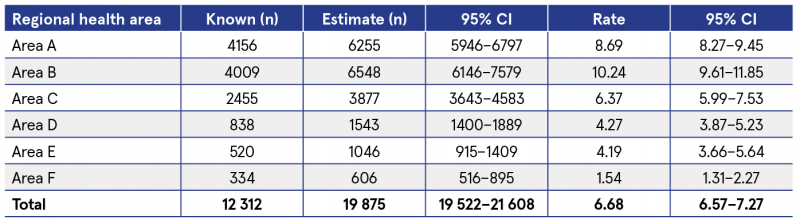
3. Estimates of problematic opioid use, 2019, by regional health area
Data on opioid use for the years 2015–2019 were collected from four sources: treatment clinics, general practitioners (GPs), the Irish Prison Service, and the Probation Service5. Employing the capture–recapture (CRC) method, Poisson log-linear models were applied to the overlap data to find the model with the best fit in order to estimate the hidden population not identified by any of the data sources. Source-by-source interaction terms were tested by adding them to the base model in all possible combinations. The best model for estimating the size of the hidden population was determined by comparing the deviance to the chi-squared distribution and the Akaike information criterion (AIC) value. The simplest model with the lowest AIC value that provided a credible estimate was used (see Table 10).
Table 10: Estimates of the number of problematic opioid users, by RHA and rates per 1,000 population aged 15–64 years, 2019
1 For further information on Sláintecare, visit:
https://www.gov.ie/en/campaigns/slaintecare-implementation-strategy/
2 Department of Health (2021) Sláintecare implementation strategy & action plan 2021–2023. Dublin: Government of Ireland. https://www.drugsandalcohol.ie/34321/
3 LINK, the NDTRS online data entry portal, will be updated by mid-2023 to automatically include these RHA and CHN, along with the existing geocodes. In the meantime, specific analysis requests can be provided on request by the NDTRS team at ndtrs@hrb.ie.
4 Ipsos MRBI (2022) The 2019–20 Irish National Drug and Alcohol Survey: technical report. Dublin: Health Research Board. https://www.drugsandalcohol.ie/36492/
5 Hanrahan MT, Millar SR, Phillips KP, Reed TE, Mongan D and Perry IJ (2022) Problematic opioid use in Ireland, 2015–2019. Dublin: Health Research Board. https://www.drugsandalcohol.ie/35856/
B Substances > Substances in general
B Substances > Alcohol
B Substances > Hallucinogens / Psychedelics
B Substances > Hallucinogens / Psychedelics > Mushrooms (psilocybin)
B Substances > Sedatives, hypnotics or tranquillisers (CNS depressants)
B Substances > Cocaine
B Substances > Cocaine > Crack cocaine
B Substances > Opioids (opiates)
B Substances > Steroids / performance image enhancing
B Substances > New (novel) psychoactive substances
HJ Treatment or recovery method > Substance disorder treatment method
HJ Treatment or recovery method > Substance disorder treatment method > Substance replacement method (substitution) > Opioid agonist treatment (methadone maintenance / buprenorphine)
J Health care, prevention, harm reduction and treatment > Risk and protective factors > Risk factors
J Health care, prevention, harm reduction and treatment > Treatment and maintenance > Treatment factors
L Social psychology and related concepts > Life circumstances
MA-ML Social science, culture and community > Risk by type of society and culture
VA Geographic area > Europe > Ireland
VA Geographic area > Europe > Ireland > County / regional data
Repository Staff Only: item control page