Lyons, Suzi  ORCID: https://orcid.org/0000-0002-4635-6673
(2024)
Trends in gabapentinoid prescribing, law enforcement, drug seizures, and postmortem toxicology in Ireland, 2010–2020.
Drugnet Ireland,
Issue 88, Summer 2024,
pp. 16-19.
ORCID: https://orcid.org/0000-0002-4635-6673
(2024)
Trends in gabapentinoid prescribing, law enforcement, drug seizures, and postmortem toxicology in Ireland, 2010–2020.
Drugnet Ireland,
Issue 88, Summer 2024,
pp. 16-19.
| Preview | Title | Contact |
|---|---|---|
|
PDF (Drugnet Ireland 88)
1MB |
Gabapentin and pregabalin are collectively known as gabapentinoids.1 They are licensed as an anti-epileptic, for neuropathic pain and generalised anxiety disorder.2 Since their market introduction (gabapentin 1993; pregabalin 2004) they have risen to become one of the most commonly prescribed medications in a number of countries. One of the theories for the rise in prescribing is the increase in off-label prescribing, i.e. being prescribed for conditions other than that licensed for, such as other pain disorders.
Of concern is that when gabapentinoids are used alongside opioids, there may be an increased risk of respiratory depression, overdose, and death. When first released onto the market, these medications were thought to have a low risk of misuse or dependence; however, ever since there has been a growing recognition of those associated risks. There has been an increased reporting of misuse or dependence to various agencies, and an increase in the number of overdose deaths where they are implicated often in combination with opioids, specifically heroin and methadone. In 2019, the United Kingdom (UK) authorities reclassified gabapentinoids as Schedule 3 (Class C) controlled drugs.
In this context, a 2024 retrospective observational study in Ireland3 aimed to:
- Describe trends in gabapentinoid prescribing (2010–2020) using General Medical Services (GMS) data from the Primary Care Reimbursement Services (PCRS)
- Examine trends in the illicit supply of gabapentinoids (2012–2020) using law enforcement data from Forensic Science Ireland and the Health Products Regulatory Authority (HPRA)
- Describe trends in the detection of gabapentinoids in a national postmortem population (2013–2020) using data from the State Laboratory, and
- Estimate rates among individuals with opioid use disorder (OUD) where gabapentinoids were found with benzodiazepines and prescription opioids using data from the State Laboratory (2013–2020).
Results
Prescribing data (2010–2020)
The prescription data include those aged 17 years and older. The analysis showed that gabapentin prescribing, after accounting for age and sex, increased every year by 6% (adjusted rate ratio (ARR) 1.06, 95% CI: 1.05–1.06, p<0.001). Gabapentin prescribing increased from 454 per 100,000 (GMS population) in December 2010, rising to a high of 823 per 100,000 in December 2020. Prescribing rates for pregabalin were greater than gabapentin for every year. In relation to demographics, women were more likely to be prescribed gabapentinoids than men. Additionally, those aged 46 years or older were more likely to be prescribed these drugs.
Drug seizure data (2012–2020)
Compared with the annual number of all drug seizures, the number of seizures of gabapentinoids is low. Gabapentin seizure numbers rarely numbered above a handful, with the highest number recorded in 2013 (n=14). Since 2016, the number of seizures of pregabalin, again while relatively low compared with the overall number of drug seizures, has been consistently higher than gabapentin, with the highest number in the study period (n=61) recorded in 2019.
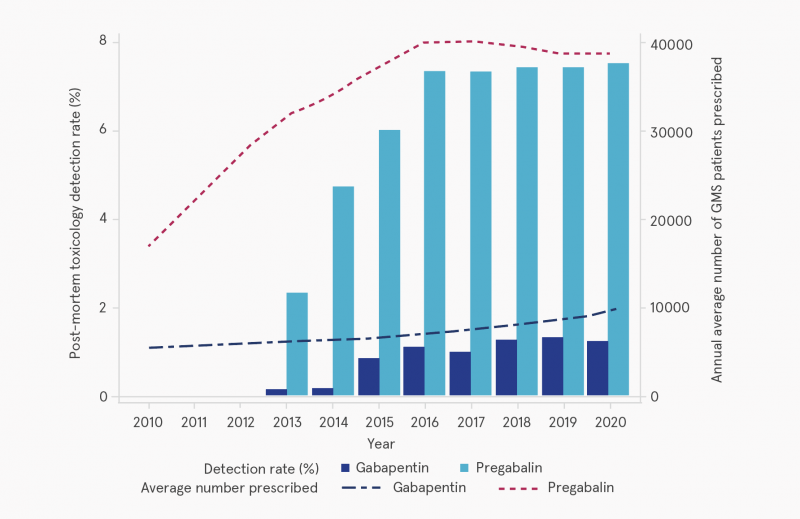
Source: Durand et al. (2024)3
The secondary y-axis shows the annual average number of patients prescribed gabapentinoids in Ireland between 2010 and 2020.
Figure 1: Postmortem toxicology detection rate for gabapentin and pregabalin in Ireland, 2013–2020
Postmortem toxicology (2013–2020)
Of the total postmortem toxicology analyses done in the study period, 1,881 (7.14%) cases tested positive for a gabapentinoid: 243 cases were positive for gabapentin (0.92%) and 1,679 (6.37%) positive for pregabalin. Both drugs were detected in a small number of cases (0.16%, n=41) (see Figure 1). There was a statistically significant increase of 28% over the 8 years in positive results, driven by the increasing numbers of pregabalin-positive results.
Rates among individuals with OUD in postmortem toxicology (2013–2020)
An individual was defined as having OUD if they tested positive for heroin or methadone in postmortem toxicology. For the period, 5.2% (n=1379) individuals tested positive for methadone and 3.2% (n=852) tested positive for heroin; in total 7.2% were classified as OUD. Of this group, 27.8% (n=528) tested positive for pregabalin compared with only 4.7% in the non-OUD group. Similar to other results, a lower number tested positive for gabapentin (n=41, 2.2%) in the OUD (compared with 0.8% in the non-OUD group). In almost 1 in 10 (8.2%) of OUD cases, benzodiazepines were found along with pregabalin, which increased over the study period, peaking at 37.3% in 2018, and then decreasing slightly to 31.3% in 2020. The proportion of OUD where benzodiazepines were found along with gabapentin was lower, but also peaked in 2018, at 3.3% before dropping to 2% in 2020.
Limitations
The study has a number of limitations. The prescription data are estimated to represent one-third of the Irish population and does not include private prescriptions or from specialist secondary care. It is likely to over-represent people with a lower socioeconomic status, women, and older people. It does not include any information about what conditions the drugs were prescribed for or other drugs prescribed along with the gabapentinoids. The number of individuals identified as OUD is likely to be underestimated due to the short half-life of heroin and its metabolite.
Discussion
The authors concluded that similar to other countries there has been an increase in gabapentinoid prescribing, in particular pregabalin, in Ireland over the last number of years. Of concern is the finding of the higher rates of pregabalin in the OUD population compared with the non-OUD population. Concurrent use of an opioid along with pregabalin can increase the risk of overdose, with some research showing that pregabalin can hinder the effectiveness of naloxone in reversing an opioid overdose.4 A number of counties have implemented regulatory measures. However, a 2023 UK study suggests that the immediate impact of reclassification of pregabalin in April 2019 in that country has been limited, particularly on prescribing for existing users of the drug,5 and had no discernible impact on English drug-related deaths for 2020.6 In September 2019, the Irish Medical Council issued an advisory notice to doctors in Ireland when prescribing pregabalin to follow best practice guidelines and only prescribe when unequivocally necessary. The authors note that this advice had no impact on pregabalin prescribing in Ireland. However, the authors also sound a note of caution, in the context of the unintended consequences in Scotland, following implementation restrictions on benzodiazepine prescribing in that jurisdiction, which resulted ultimately in an increase in drug-related deaths.7
The authors conclude that their findings raise concerns about the risk of ubiquitous prescribing of pregabalin in Ireland, associated street supply, and in particular the potential serious harmful consequences to people who are also using opioids.
1 Neurontin is a common brand name for gabapentin, while Lyrica is a common brand name for pregabalin.
2 Pregabalin is licensed for fibromyalgia in the United States only.
3 Durand L, O’Kane A, Tierney J, et al. (2024) Gabapentinoids in Ireland 2010 to 2020: an observational study of trends in gabapentinoid prescribing, law enforcement drug seizures and postmortem toxicology. Br J Clin Pharmacol, 90(4): 987–995. Available from: https://www.drugsandalcohol.ie/40133/
4 Lyndon A, Audrey S, Wells C, et al. (2017) Risk to heroin users of polydrug use of pregabalin or gabapentin. Addiction, 112(9): 1580–1589. Available from: https://www.drugsandalcohol.ie/34645/
5 Ashworth J, Bajpai R, Muller S, et al. (2023). Trends in gabapentinoid prescribing in UK primary care using the Clinical Practice Research Datalink: an observational study. Lancet Reg Health Eur, 27: 100579.
6 Kalk NJ, Chiu CT, Sadoughi R, et al. (2022) Fatalities associated with gabapentinoids in England (2004–2020). Br J Clin Pharmacol, 88(8): 3911–3917.
7 McAuley A, Matheson C and Robertson JR (2022). From the clinic to the street: the changing role of benzodiazepines in the Scottish overdose epidemic. Int J Drug Policy, 100: 103512.
E Concepts in biomedical areas > Medical substance > Prescription drug (medicine / medication)
HJ Treatment or recovery method > Substance disorder treatment method > Substance disorder drug therapy (pharmacological treatment)
MM-MO Crime and law > Substance related offence > Drug offence > Illegal drug possession (seizures)
P Demography, epidemiology, and history > Population dynamics > Substance related mortality / death
VA Geographic area > Europe > Ireland
Repository Staff Only: item control page