Fanagan, Sarah (2016) Suicide and untimely sudden deaths in the Donegal Mental Health Service. Drugnet Ireland, Issue 59, Autumn 2016, pp. 16-17.
| Preview | Title | Contact |
|---|---|---|
|
PDF (Drugnet 59)
1MB |
In 2014, the HSE Donegal Mental Health Service (DMHS) commissioned a study which sought insight into an increasing number of premature deaths among its service users.1 The research, which was funded by the National Office for Suicide Prevention (NOSP) and conducted by a team from the National Suicide Research Foundation (NSRF), examined 34 deaths among those in the care of the DMHS between October 2011 and May 2015. The study has produced a number of evidence-based recommendations to improve the assessment and management of people at risk of suicidal behaviour in a mental health service setting.
Suicide Support and Information System–Psychological Autopsy Model
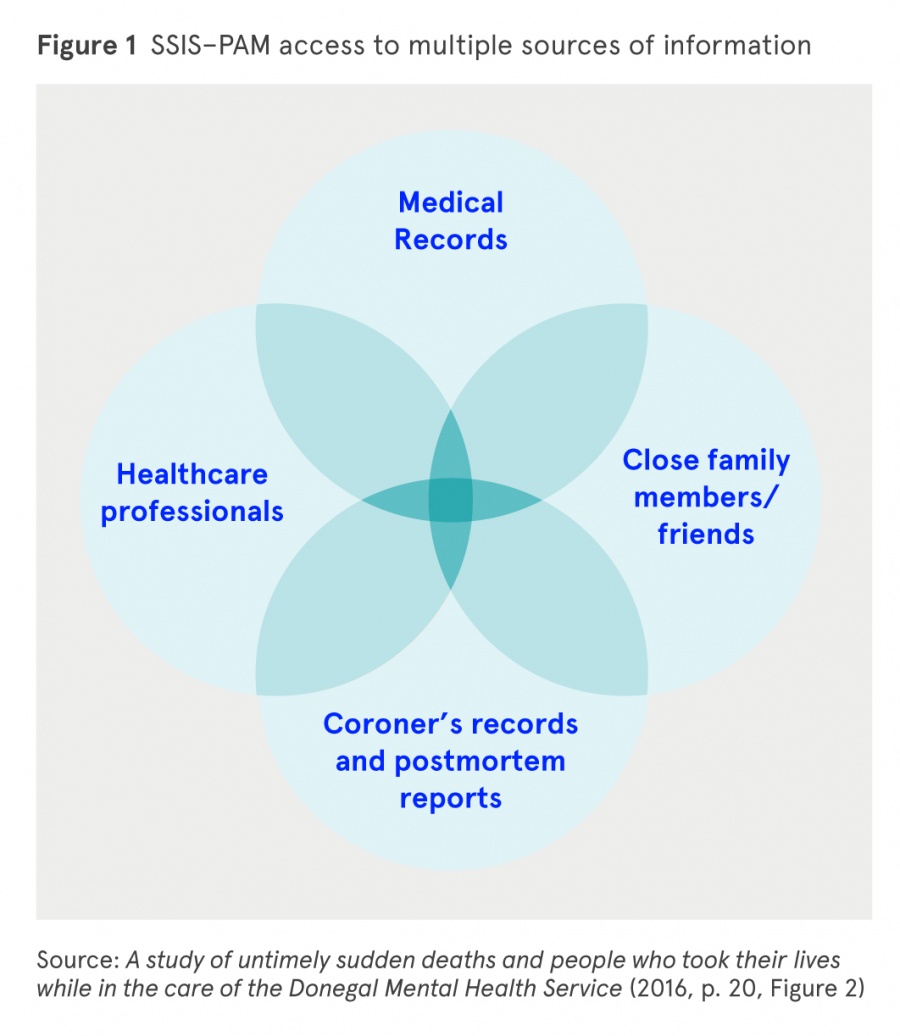
The Suicide Support and Information System–Psychological Autopsy Model (SSIS–PAM) used in this study was developed to prevent suicide by proactively facilitating access to support for the bereaved, while at the same time obtaining information on risk factors associated with suicide and deaths classified as open verdicts. Data were collected from multiple sources to corroborate the clinical history of the deceased as well as offering support to family members following such a tragic event. Twenty-four family informant interviews were conducted, with 21 families providing consent for the researchers to contact GPs involved in the care of the deceased. Thirteen GPs completed and returned questionnaires.
Recording of deaths
The recording of suicide and sudden unexpected deaths that may have been the result of suicidal or self-harming behaviour poses challenges to understanding the true incidence of suicide in a community at a particular time, as official figures are measured by calendar year and remain provisional for up to two years post-event. This research has provided DMHS with a ‘real time’ database with information on sociodemographic, psychosocial and psychiatric risk factors that may have contributed to the untimely deaths or suicides of those in its care over the period considered. The maintenance of this data will inform policy and resource planning and facilitate a targeted response to suicide contagion and emerging suicide clusters.
Key findings
Of the 34 deaths examined:
- 67.8% were men.
- The men were younger than the women, with mean ages of 41.4 years and 44 years, respectively.
- Clinical files showed cause of death as overdose of medication or drugs (n=15, 44%), hanging (n=14, 41%) and drowning (n=5, 15%).
- Of those who died by intentional overdose, the majority involved prescribed medication, with toxicology results of 10 cases also indicating substantial amounts of alcohol in both blood and urine at time of death. Most recent figures from the National Drug-Related Deaths Index (NDRDI) show that two-fifths (41%) of poisonings in 2013 involved benzodiazepines.2
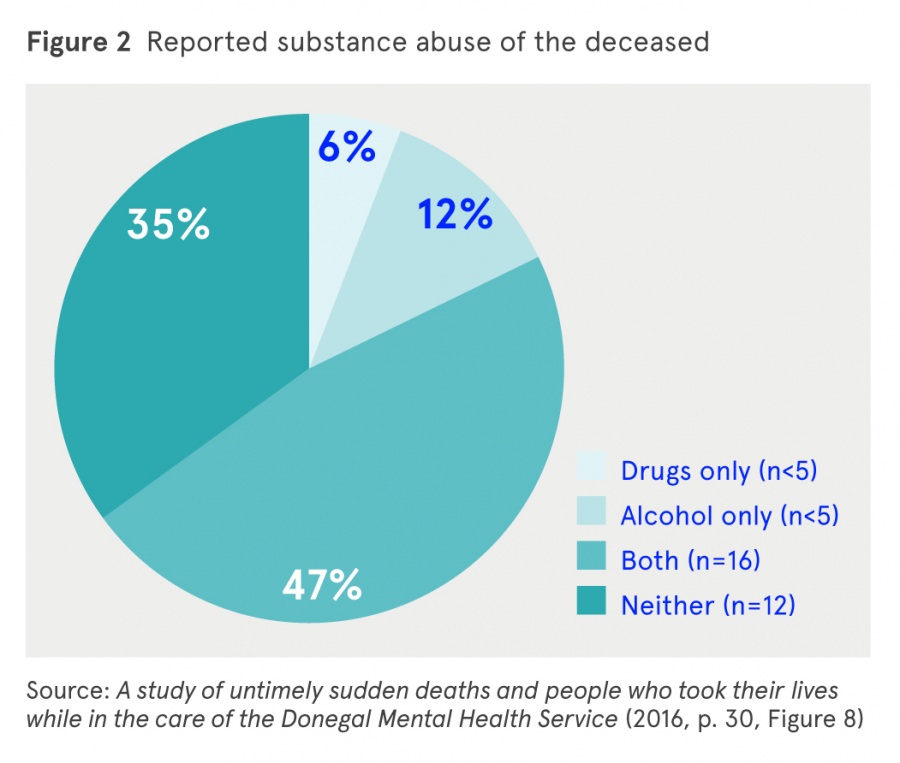
- Almost half were known to abuse both drugs and alcohol prior to death (n=16, 47%) and a further six had abusive or dependent issues with a single substance.
- 76.5% had a history of self-harm (n=26).
- The majority had a history of at least one voluntary or involuntary inpatient psychiatric admission (n=31).
- Psychiatric diagnosis was confirmed in all 34 cases, with 85% also meeting criteria for a secondary disorder; 47% had a primary diagnosis of depressive disorder (n=16) and a secondary diagnosis of substance abuse was recorded in 47% of cases.
- 82% were being prescribed medication for mental illness preceding death. Information gathered on these cases included reckless behaviour, such as hoarding large supplies while requesting repeat prescriptions, and selling or exchanging prescribed medication for illegal drugs.
- The majority (n=18) had family members with known mental health issues, with depression and substance abuse the most common.
- 44% of case files contained incomplete assessments of suicidal risk, which was recorded in a way that was not considered to be informative of the service user’s suicidal state. In 56% of case files, appropriate evaluation was conducted and made available in accordance with best practice principles.
Media reporting of suicides and unexpected sudden deaths
The National Media Monitoring Agency conducted a search of media outlets in County Donegal and nationally to determine the extent of media reporting of the cases of suicide and probable suicide examined in this study covering the period January 2011 to March 2015.
- Overall, journalistic reporting was mindful of the effect that over sensationalised reports can have on family and friends of the deceased and wider community.
Recommendations
The study makes six recommendations, covering 19 actions, based on its findings in relation to the characteristics of the deceased, patterns regarding contact with mental health services, and the needs of families bereaved by suicide. These can be summarised as follows:
- Improve clinical practice to increase understanding among mental health service staff about service user suicide and self-harm risk that is mindful of gender, age and other factors (such as cases of dual diagnosis) which may influence the risk of premature death.
- Prioritise uniformity of good practice.
- Foster communication and engagement with family members.
- Improve the service response to family members following the death of a service user.
- Improve media reporting of suicide.
- Implement the Suicide Support and Information System.
According to Dr Clifford Haley, Executive Clinical Director, Donegal Mental Health Services: ‘This data set of consecutive untimely sudden deaths will contribute to suicide research internationally, but most importantly it helps cast light onto what must be done to provide effective suicide prevention in Ireland.’
1 Corry C, Arensman E and Williamson E (2016) A study of untimely sudden deaths and people who took their lives while in the care of the Donegal Mental Health Service. Cork: National Suicide Research Foundation. https://www.drugsandalcohol.ie/25727/
2 Health Research Board (2015) Drug-related deaths and deaths among drug users in Ireland: 2013 figures from the National Drug-Related Deaths Index. Dublin: Health Research Board. https://www.drugsandalcohol.ie/24676
G Health and disease > State of health > Mental health
J Health care, prevention, harm reduction and treatment > Type of care > Mental health care (Psychiatry / Psychology)
P Demography, epidemiology, and history > Population dynamics > Substance related mortality / death
VA Geographic area > Europe > Ireland > Donegal
Repository Staff Only: item control page