Doyle, Anne (2021) Alcohol consumption, alcohol-related harm, and alcohol policy in Ireland. Drugnet Ireland, Issue 78, Summer 2021, pp. 1-8.
| Preview | Title | Contact |
|---|---|---|
|
PDF (Drugnet Ireland 78)
1MB |
The Health Research Board (HRB) Alcohol Overview was published in April 2021, the fourth in a series that provides updates on alcohol consumption, its related harms, and policy responses in Ireland.1 Using the HRB National Drugs Library, the overview is compiled using a variety of Irish data sources, published Irish literature, and existing information systems and surveys.

Introduction
Alcohol use is the seventh leading risk factor for both deaths and disability-adjusted life years globally, despite the fact that one-half of the world’s population does not drink. Ireland ranks ninth highest per capita alcohol consumption of all OECD (Organisation for Economic Co-operation and Development) member countries.2
Alcohol consumption
Since 2013, alcohol consumption levels in Ireland have remained stable but high: 19% higher than the stated aim of the Irish Government to reduce per capita alcohol consumption in Ireland to 9.1 litres by 2020. In 2019, per capita alcohol consumption per adult aged 15 and over was 10.8 litres of pure alcohol (see Figure 1).3,4,5 However, considering that one-quarter of the population do not drink alcohol at all, the number of litres consumed per person is even greater.

Consumption patterns
Patterns of alcohol consumption as well as high-volume drinking increases the risk of alcohol-related harm. Healthy Ireland Survey data showed that more than one-half (52%) of all drinkers were classified as hazardous drinkers using the World Health Organization’s AUDIT-C screening tool.6 This screening tool takes account of frequency and volume of drinking as well as heavy episodic drinking (HED), defined as consuming six standard drinks or more on a single drinking occasion. Hazardous drinking was more common among men (70%) than women (34%), particularly younger men, with almost four in five (78%) of 25–34-year-old males meeting the criteria for hazardous drinking.7
Despite the level of hazardous drinking patterns among Irish drinkers, the majority of drinkers considered themselves as being a light or moderate drinker (74%), indicating an unawareness of what constitutes binge drinking and that their patterns of drinking may be considered hazardous.
Alcohol consumption among young people
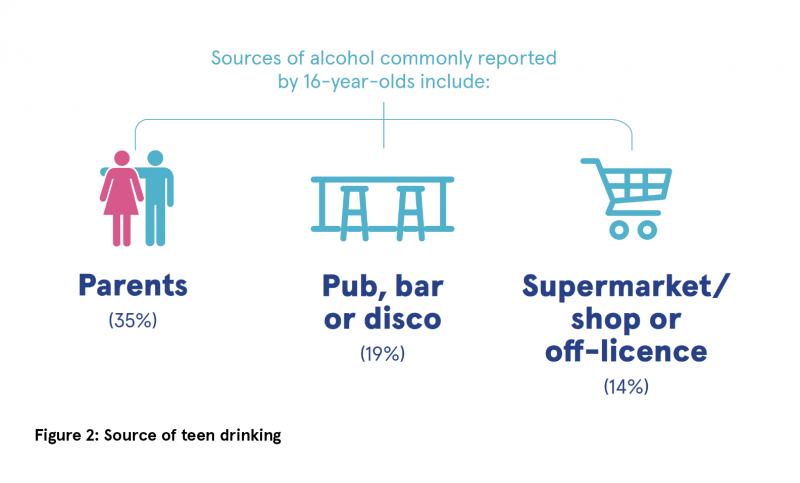
Data from the Irish Health Behaviour in School-aged Children (HBSC) 2018 study indicate that 82% of schoolchildren have consumed their first alcoholic drink by the age of 17 years and for all ages, with the exception of 15-year-olds, getting alcohol from parents and guardians was the most common way children obtained alcohol (see Figure 2).8 Lifetime drunkenness ranged from 5% of 13-year-olds to 62% of 17-year-olds. Trends in alcohol consumption since 1998 show a continuous decline in the percentage of schoolchildren who drink alcohol, especially among 13–15-year-olds. This is encouraging, as this group is particularly vulnerable to experiencing alcohol-related harm. The same trend has not been observed among 17-year-olds, where there has been little change in alcohol use and drunkenness since 1998.
Alcohol consumption among parents
More than one-quarter of parents (28%) engaged in HED at least once a month, while 5% were classified as dependent on alcohol.6
Alcohol-related harm in Ireland
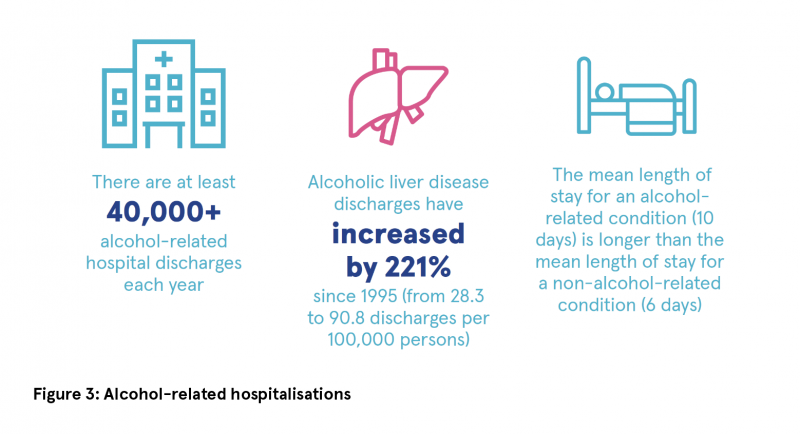
The Hospital In-Patient Enquiry (HIPE) scheme collects clinical and administrative data on discharges (including deaths) from acute Irish hospitals. For the overview, all alcohol-related discharges that were either wholly attributable to alcohol (alcohol is a necessary cause for these conditions to manifest) or partially attributable (conditions where alcohol may be one of a range of causative factors) were analysed (see Figure 3).
Wholly attributable alcohol-related discharges
In 2018, acute conditions such as alcohol poisoning and intoxication accounted for 12% of wholly attributable alcohol-related discharges. Chronic diseases, such as liver disease, accounted for 23% of such discharges, while other chronic conditions, including alcohol dependence, accounted for 64%. Acute alcohol-related conditions were more common among younger people, whereas chronic diseases and other chronic conditions were more prevalent among the older age groups.
Alcoholic liver disease discharges
The number of discharges with a diagnosis of alcoholic liver disease has increased by 221% since 1995, to 90.8 per 100,000 persons. The increase was most pronounced among those aged 15–34 years and those aged 65 years or over. Of all discharges with a diagnosis of alcoholic liver disease, 8.4% died while in hospital.
Partially alcohol-attributable conditions
Between 2012 and 2017, there were 121,919 hospital discharges from partially alcohol-attributable conditions. In 2017, there were 20,201 hospital discharges due to partially alcohol-attributable conditions.
Males accounted for 87% of these discharges. Although females accounted for just 13% of all partially alcohol-attributable hospital discharges in 2017, more than one-third (37%) of alcohol attributable cancer discharges were female. This is primarily due to the high number of breast cancer discharges related to alcohol. The number of partially alcohol-attributable hospital discharges reported in this overview represent the minimum number of hospital discharges related to alcohol use; the true number is likely to be considerably higher.
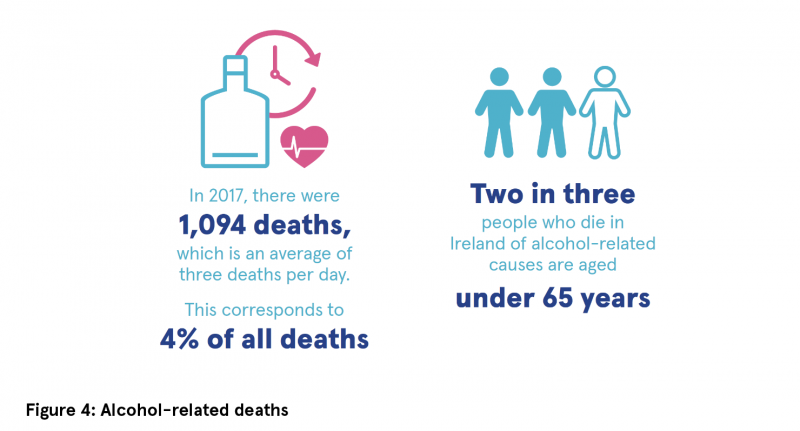
Alcohol mortality
Between 2008 and 2017, there were 10,803 alcohol-related deaths recorded on the National Drug-Related Deaths Index (NDRDI): 8,000 male and 2,803 female. In 2017, there were 1,094 deaths recorded (see Figure 4).
In 2018, some 30% of self-harm cases were alcohol related. Alcohol was significantly more common in male presentations of self-harm (34%) compared with female presentations (27%). It was also associated with peaks in hospital attendances at night, at weekends, and on public holidays.
Alcohol treatment
Between 2013 and 2019, some 53,200 cases were recorded on the National Drug Treatment Reporting System (NDTRS) as attending for treatment with alcohol as their main problem drug. Those registered on the National Psychiatric Inpatient Reporting System (NPIRS) as attending psychiatric inpatient treatment for alcohol dependence has decreased by over 60% from 2006 (2,767 cases) to 2019 (1,090 cases), largely due to a move to outpatient settings for such treatment.
Alcohol policy response in Ireland
Since the most recent overview in 2016, the most important development in alcohol policy in Ireland has been the enactment of the Public Health (Alcohol) Act 2018. The main provisions of the Act include:
· Minimum unit price (MUP): A minimum price set at 10 cent per gram of alcohol in the product is compulsory.
· Structural separation of alcohol products: Physically separating alcohol products from other grocery items is compulsory.
· Restrictions around alcohol advertising: Restricting content of advertisements, involving a 9pm broadcast watershed for advertisements on television and radio; a ban on advertising alcohol products near schools, in parks, on public transport, in train and bus stations, and at bus or Luas stops are compulsory.
· Labelling of alcohol products: Labelling the direct link between alcohol and cancer; the number of grams of alcohol in the container; the calorie content; and details of a Health Service Executive (HSE) website providing public health information are compulsory. Health warning labels on alcohol products are subject to scrutiny at European Union (EU) level and have yet to be commenced.
Conclusion
Since the last Alcohol Overview was published in 2016, little has changed with regard to alcohol consumption and alcohol-related harm. Ireland still has a high level of per capita consumption and a majority of drinkers in Ireland consume alcohol in a manner risky to their health. The consequences of drinking patterns in Ireland are reflected in the mortality data, which show that on average there have been three alcohol-related deaths every day since 2008. The signing into law of the Public Health (Alcohol) Act in 2018 was an important first step in reducing alcohol-related harm; however, for real impact, the remaining sections need to be implemented in full as soon as possible.
1 O’Dwyer C, Mongan D, Doyle A and Galvin B (2021) Alcohol consumption, alcohol-related harm and alcohol policy in Ireland. HRB Overview Series 11. Dublin: Health Research Board.
https://www.drugsandalcohol.ie/33909/
2 Organisation for Economic Co-operation and Development (OECD) (2019) Alcohol consumption. Available online at: https://data.oecd.org/healthrisk/alcohol-consumption.htm (accessed 20/12/2019)
3 Revenue Commissioners (2019) Excise receipts by commodity. Dublin: Office of the Revenue Commissioners. Available online at:
https://www.revenue.ie/en/corporate/information-about-revenue/statistics/excise/receipts-volume-and-price/excise-receipts-commodity.aspx
4 Central Statistics Office (2019) Population and migration estimates April 2019. Cork: Central Statistics Office. Available online at:
https://www.cso.ie/en/releasesandpublications/er/pme/populationandmigrationestimatesapril2019/
5 Central Statistics Office (2017) Census 2016 profile 3 – an age profile of Ireland. Cork: Central Statistics Office. Available online at:
https://www.cso.ie/en/csolatestnews/presspages/2017/census2016profile3-anageprofileofireland/
6 Ipsos MRBI (2017) Healthy Ireland Survey 2017. Dublin: Department of Health.
https://www.drugsandalcohol.ie/28041/
7 National Advisory Committee on Drugs and Alcohol/Department of Health (UK) (2016) Prevalence of drug use and gambling in Ireland and drug use in Northern Ireland. Bulletin 1. Dublin: National Advisory Committee on Drugs and Alcohol. https://www.drugsandalcohol.ie/26364/
8 Költő A, Gavin A, Molcho M, Kelly C, Walker L and Nic Gabhainn S (2020) The Irish Health Behaviour in School-aged Children (HBSC) Study 2018. Dublin: Department of Health & Health Promotion Research Centre, National University of Ireland Galway. https://www.drugsandalcohol.ie/31531/
A Substance use and dependence > Prevalence > Substance use behaviour > Alcohol consumption
A Substance use and dependence > Substance related societal (social) problems
B Substances > Alcohol
G Health and disease > Substance use disorder (addiction) > Alcohol use disorder
J Health care, prevention, harm reduction and treatment > Health related issues > Health information and education > Health labels / labelling
J Health care, prevention, harm reduction and treatment > Treatment and maintenance > Treatment factors
MP-MR Policy, planning, economics, work and social services > Policy > Policy on substance use
VA Geographic area > Europe > Ireland
Repository Staff Only: item control page