Thiemt, Britta (2020) Oral fluid testing for methadone maintenance patients – accuracy and acceptability. Drugnet Ireland, Issue 73, Spring 2020, pp. 20-21.
| Preview | Title | Contact |
|---|---|---|
|
PDF (Drugnet Ireland 73)
758kB |
Methadone maintenance treatment is an addiction treatment provided to about 10,000 people in Ireland to improve their health and stability.1 In a 2019 study published in the Irish Journal of Medical Science, O’Callaghan et al.2 investigated how accurate and acceptable oral fluid testing is to methadone maintenance patients and doctors as a means of substance detection. Importantly, this was the first Irish study capturing patient views on their experience with methadone maintenance.
Background
According to the authors, drug testing during methadone maintenance is crucial as it provides doctors with important insights into patient stability and contributes to decisions about the level, frequency, and supervision of methadone delivery. In Ireland, unsupervised urine testing is commonly used and preferred by general practitioners (GPs). However, unsupervised urine samples can be subject to falsification, and the 2010 external review of the Irish Methadone Maintenance Treatment Protocol3 called for discontinuing supervised urine testing due to its inherent infringement of patient privacy. Testing oral fluid rather than urine is an alternative method for detecting drug metabolites under supervision, without compromising patient privacy. However, its window of detection is shorter than that of urine testing. Hence, the current study examined how accurately oral fluid testing could detect drug metabolites in comparison with urine testing and self-report. It also investigated patients’ and doctors’ views on the acceptability of each method and on methadone maintenance generally.
Methods
The study was carried out with seven GPs from four practices within the GP training scheme of Trinity College Dublin and the Health Service Executive from January to April 2016. Of the 65 invited patients, 55 (85%) agreed to participate. The average age of participants was 42.5 years and about two-thirds were male. The authors compared how many patients in the sample (n=55) were identified as having consumed a substance by means of (a) unsupervised urine testing, (b) supervised oral fluid testing, and (c) self-report. Patient views were captured with an eight-item questionnaire administered by GPs.
Key findings
Accuracy
For most drugs, results from oral fluid testing were similar to those from urine testing, with the exception of benzodiazepines (see Figure 1).
Methadone: Consumption of methadone was confirmed through all three methods for all patients (n=55).
Benzodiazepines: Detection of benzodiazepines was superior in urine testing (n=41) and self-report (n=37) compared with oral fluid testing (n=18).
Opiates: Detection of opiates was highest by means of self-report (n=16), and much lower both through urine (n=3) and oral fluid testing (n=5). Additionally, only self-report could identify the type of opiate (heroin n=3; painkillers n=13).
Cocaine and amphetamines: Self-report was superior in capturing cocaine consumption (n=6) compared with both urine (n=2) and oral fluid testing (n=1). Only one patient self-identified as having consumed amphetamines, which was picked up by neither urine nor oral fluid testing.
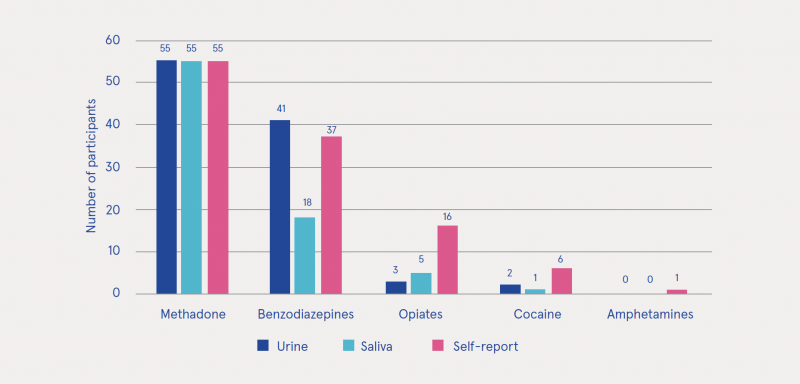
Figure 1: Drug testing results by each of the three methods (n=55)
Acceptability
Views: Most patients (95%) and the seven participating GPs evaluated oral fluid testing as acceptable and straightforward, with 60% of patients preferring oral fluid testing, but 13% preferring urine testing.
Time and reliability: GPs noted that additional time was necessary to perform both tests; three of them stressed the lack of reliability in the detection of benzodiazepines through oral fluid testing.
Urine sample supervision: Contrary to author expectations, only 15% of patients were against supervised urine samples. The authors attributed this to potential reluctance among patients to express negative views to their doctors directly, as well as possible altered levels of self-esteem and expectations for privacy for methadone patients.
Patient experience of methadone maintenance
Positive vs negative views: Overall, negative views of methadone maintenance were more frequent than positive ones among the patient sample.
Detoxification: More options for detoxing off methadone were desired by 20% of patients.
Positive perceptions: Perceived positive aspects included methadone allowing for stabilisation (28%), an alternative to drug use (25%), and better functioning (18%).
Negative perceptions: Perceived negative aspects included methadone being addictive (30%), associated with stigma (12%), a long-term treatment (11%), causing dental issues (11%), and causing physical side-effects (10%).
Discussion and conclusions
The current study found that, for most drugs, results from oral fluid testing were similar to those from urine testing but inferior for benzodiazepines. O’Callaghan et al. attributed this to the longer window of detection of benzodiazepines in urine compared with oral fluid. However, while many participants reported using benzodiazepines (67%), the authors state that 61% had a prescription for them, drawing into question the importance of their detectability. Hence, the authors conclude that oral fluid testing is an acceptable addition for drug screening in methadone maintenance treatment, and especially advantageous if a urine sample cannot be supplied. Additionally, they found that self-report as a measure of concomitant drug use was as or more worthwhile compared with urine or saliva testing.
However, the authors suggest that studies with larger samples are necessary to further investigate the detectability of drugs through oral fluid testing, especially when considering the low number of patients recorded as having consumed cocaine and amphetamines (through self-report or testing). Overall, given the increasing drug-related mortality observed in Ireland, the authors stress the importance of more research on the substance use but also the perspectives and experiences of methadone maintenance patients.
1 Delargy I, Crowley D and Van Hout MC (2019) Twenty years of the methadone treatment protocol in Ireland: reflections on the role of general practice. Harm Reduct J, 16(1): 5. https://www.drugsandalcohol.ie/30173/
2 O’Callaghan ME, Regan L, Wilson M, Byrne E, Hollywood B, O’Kelly F, et al. (2020) Acceptability and accuracy of oral fluid drug testing for patients on methadone maintenance. Ir J Med Sci, 189: 557–561. https://www.drugsandalcohol.ie/31236/
3 Farrell M and Barry J (2010) The introduction of the opioid treatment protocol. Dublin: Health Service Executive. https://www.drugsandalcohol.ie/14458/
HJ Treatment or recovery method > Substance disorder treatment method > Substance replacement method (substitution) > Opioid agonist treatment (methadone maintenance / buprenorphine)
HJ Treatment or recovery method > Treatment outcome
J Health care, prevention, harm reduction and treatment > Identification and screening > Identification and screening for substance use
J Health care, prevention, harm reduction and treatment > Treatment and maintenance > Treatment factors
J Health care, prevention, harm reduction and treatment > Treatment and maintenance > Patient / client attitude toward treatment (experience)
VA Geographic area > Europe > Ireland
Repository Staff Only: item control page