Galvin, Brian (2019) HRB evidence review on dual diagnosis treatment service. Drugnet Ireland, Issue 69, Spring 2019, pp. 3-5.
| Preview | Title | Contact |
|---|---|---|
|
PDF (Drugnet Ireland 69)
1MB |
The Health Research Board (HRB) recently published a review entitled Treatment services for people with co-occurring substance use and mental health problems: a rapid realist synthesis.1 This report is part of the HRB Drug and Alcohol Evidence Review series and was undertaken by a team from the Georgia Health Policy Center. The three initial research questions guiding the review were:
- What interventions improve treatment and personal functioning outcomes for people with co-occurring substance use and mental health problems and in what circumstances do they work?
- What aspects of integrative programmes for the treatment of co-occurring substance use and mental health problems trigger positive system outcomes and in what circumstances do these outcomes occur?
- What existing models of care for adults with co-occurring substance use and mental health problems lead to positive treatment outcomes and successful service integration?
A number of systematic reviews have examined interventions responding to specific mental health conditions or substances. These reviews were limited as they focused on particular substances or particular mental health conditions. While the evidence suggests that greater integration of mental health and addiction services leads to improved treatment outcomes, recent studies from the United States suggest that the capacity of services to provide an effective response for clients with co-occurring problems is very limited. The purpose of the HRB realist review was to understand what aspects of the integrative process made it more likely that better treatment outcomes would be achieved. In other words, how can we get an understanding of what works for whom in what circumstances so that the integration of services benefits the users of these services.
The HRB asked the review team to take a realist approach to studying the literature on the topic. This means that they sought to identify the characteristics, or mechanisms, that are more likely to result in successful implementation of evidence-based treatments and the contexts in which this change occurs. An important aspect of the realist approach is to understand the context in which service providers and others will benefit from the knowledge contained in the review. The review team met with a number of knowledge users at an early point in the review process and, based on a thematic analysis of the discussions at these meetings, it generated 10 theory statements to guide the literature search, data extraction, and analysis (see Table 1). This theory-driven approach is an essential part of the realist synthesis process.
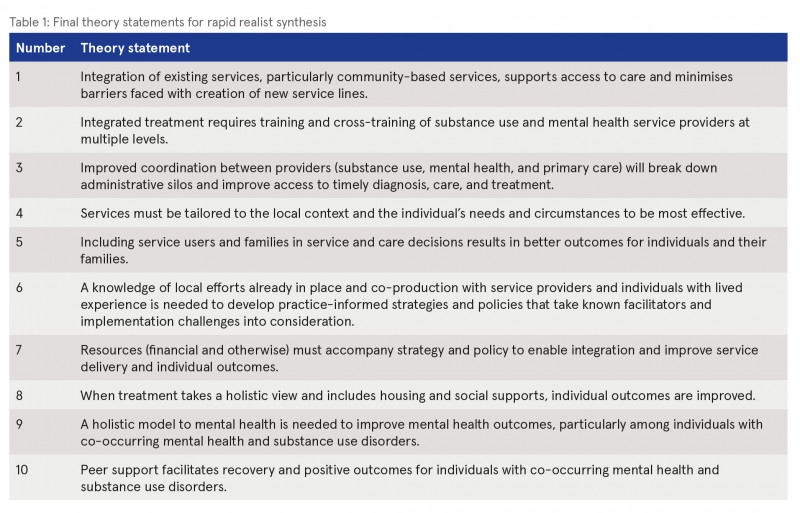
The literature search involved two stages, the first concentrating on studies on mental health and substance use treatment, integration of health programmes and services, and articles on integrated dual diagnosis models of care. The second stage broadened the search and looked for studies relevant to the topics of peer support, inclusion in service and care decisions, and recognition of the value of lived experience. The review team synthesised the data from the selected articles and aligned the context, mechanism, and outcomes found in the literature with each research question. The 10 theory statements were grouped into outcome areas of integration, access, and individual and family treatment outcomes, and the findings of the review are presented by these outcome areas.
Main findings
Integration
Each of the three outcome areas is associated with a different context. The mechanisms in improved integration are associated with the provider context. Alignment of organisational and financial resources with strategy and policy is needed for integration of services but it does not guarantee success. A culture of hope and an empowering collaborative climate help to build providers’ confidence in their ability to implement changes in services and to address the needs of those with comorbid problems. Providers’ belief that change is possible and enthusiasm for implementing these changes serve as catalysts for the change that integrated care requires. Staff confidence and hope is also developed when training is delivered in an environment that supports co-production and values the knowledge of individuals with lived experience.
When financial resources are applied in an empowering collaborative climate, formal partnerships can be developed across organisations and an open dialogue supporting a common language can develop. In this atmosphere, intermediary outcomes, such as unified case management, coordination of care, and shared treatment plans, are more likely to result and enable better integration of services.
Access
The context in relation to access mechanisms is mental health or substance use services undergoing change and seeking to work with providers of different kinds of services. In this context, staff knowledge and increased confidence related to training is associated with prompt diagnosis and consequently increased access to treatment. Staff adoption of a client-centred approach and displays of kindness are associated with increased patient engagement.
Individual and family treatment outcomes
The context for this category of outcomes is the care setting. A dominant theme under this category is the importance of engagement in treatment. Conditions that are associated with engagement are a supportive social network, progress in self-management behaviours, and stability in basic social and employment needs. A care system that works with the individual to establish a secure and stable environment makes engagement in treatment and recovery more likely.
The literature also reveals three more difficult-to-observe mechanisms that are part of this complex system: trust, flexibility, and hope. There are specific actions and orientations that contribute to trust. For example, creating an environment that is intentional about displaying simple acts of kindness will help build trust. Purposefully building flexibility into treatment through co-design will help build the conditions necessary for recovery. Building a culture of hope among providers, family, and clients through instilling confidence, self-esteem, and empowerment is critical to recovery.
Initial recommendations
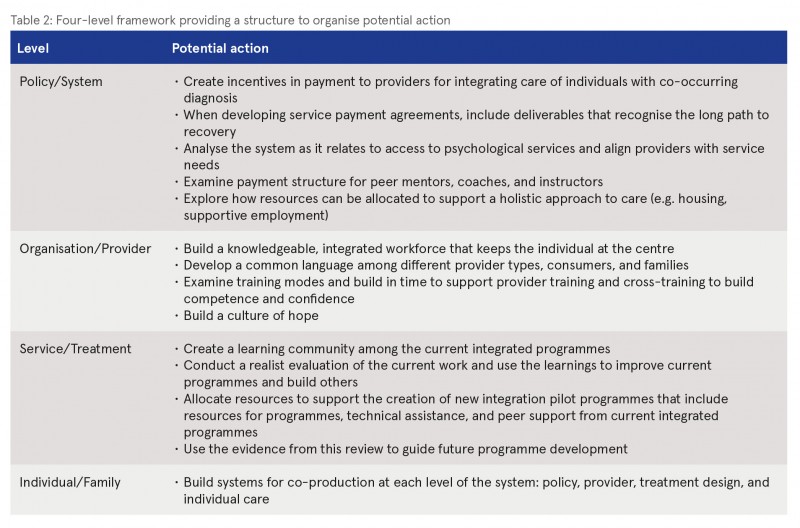
The findings of this realist review and the wisdom gained from local knowledge users provide ideas on how to build an integrated system. Local integrated programmes provide a starting place for learning and integrating knowledge about treatment and building a culture of co-production that supports putting the individual at the centre of the system. The four-level framework that emerged from this project provides a structure to organise potential steps (see Table 2). At the policy/system level, high-leverage steps may focus on the alignment of resources. At the organisation/provider level, a focus on building a knowledgeable workforce is important. Initial recommendations, included in the table for each level, are focused on a few preliminary actions that may have high leverage and build on what currently exists. A next useful step could be a collaborative session with local Irish knowledge users to meaningfully mine the findings for appropriate actions and would be in keeping with the co-production recommendation.
Conclusion
The realist review and synthesis begins to answer the overarching question of how can integration using effective models of care improve outcomes for individuals with co-occurring mental health and substance use disorders? Integration is not a single concept related to a specific treatment or relationship among providers, but rather a complex, multifaceted portfolio of interrelated parts of a system. Central to the development of integrated models is a four-level framework for integration that is co-produced by policymakers, providers, and clients at the policy, organisation or provider, treatment, and individual levels. Policies and resources need to be aligned to create incentives for providing integrated care, while a knowledgeable, coordinated workforce keeps the individual at the centre.
- Minyard K, Manteuffel B, Smith CM, Attell BK, Landers G, Schlanger M and Dore E (2019) Treatment Services for people with co-occurring substance use and mental health problems. A rapid realist synthesis. HRB Drug and Alcohol Evidence Review 6. Dublin: Health Research Board https://www.drugsandalcohol.ie/30376
G Health and disease > Substance related disorder > Substance related mental health disorder > Dual diagnosis / comorbidity (mental health)
J Health care, prevention, harm reduction and treatment > Treatment and maintenance > Treatment factors
J Health care, prevention, harm reduction and treatment > Health care delivery
VA Geographic area > Europe > Ireland
Repository Staff Only: item control page