Curtin, Margaret (2016) National Registry of Deliberate Self-Harm - annual report 2014 . Drugnet Ireland, Issue 58, Summer 2016, pp. 16-17.
| Preview | Title | Contact |
|---|---|---|
|
PDF (Drugnet 58)
745kB |
The 13th annual report from the National Registry of Deliberate Self-Harm was published in September 2015.1 The report contains information relating to every recorded presentation of deliberate self-harm to acute hospital emergency departments in Ireland in 2014, and complete national coverage of cases treated. All individuals who were alive on admission to hospital following deliberate self-harm are included, along with the methods of deliberate self-harm that were used. Accidental overdoses of medication, street drugs or alcohol are not included.
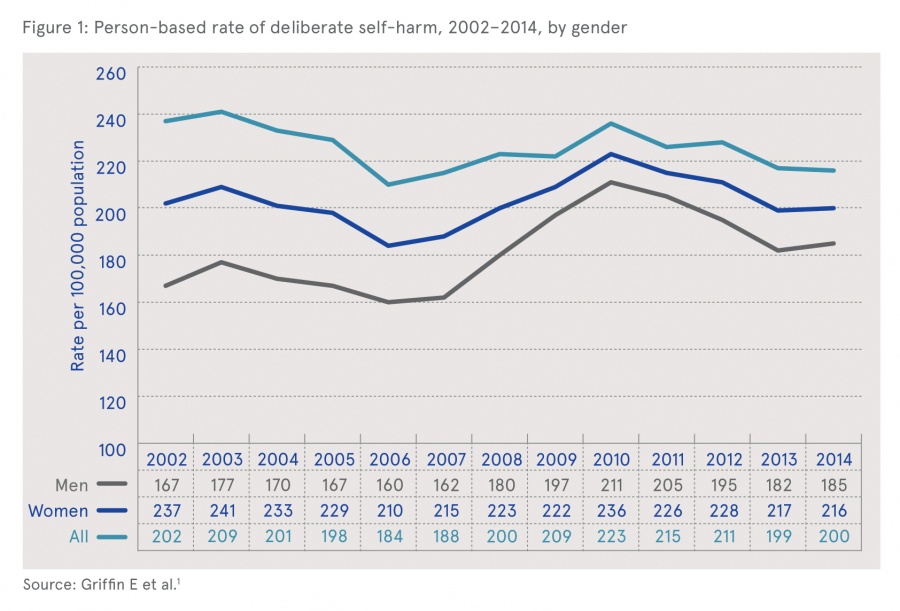
There were 11,126 recorded presentations of deliberate self-harm, involving 8,708 individuals, in 2014. This implies that more than one in five (2,418, 22%) of the presentations were repeat episodes. There was virtually no change in the rate of presentations between 2013 and 2014, following a 6 per cent decrease between 2012 and 2013. The rate in 2014 remained 6 per cent higher than the pre-recession rate of 188/100,000 in 2007 (Figure 1). The only age group in which there was significant change in the rate of deliberate self-harm between 2013 and 2014 was boys aged 10 to 14 years, among whom the rate increased by 44 per cent, from 34 to 49 per 100,000.
Forty-six per cent of self-harm presentations in 2014 were men, and just over half (54%) were aged under 30 years. People living in hostels for the homeless or of no fixed abode made up 5 per cent (n=514) of self-harm presentations. Presentations peaked in the hours around midnight and were highest on Sundays and Mondays, with 31 per cent of episodes occurring on these two days. There was evidence of alcohol consumption in 3,860 (35%) presentations and this was more common among men (37%) than women (33%).
Drug overdose was the most common form of deliberate self-harm reported in 2014, occurring in 7,314 (66%) episodes. This was a small decrease (-2%) on 2013. Overdose rates were higher among women (72%) than among men (58%). In 70 per cent of cases the total number of tablets taken was known, with an average of 28 tablets taken in these episodes. A minor tranquilliser (most commonly benzodiazepines) was involved in 37 per cent of all drug overdoses; 28 per cent of overdoses involved paracetamol-containing medicines; 21% involved antidepressants or mood stabilisers (most commonly selective serotonin reuptake inhibitors [SSRIs]); 10 per cent involved a major tranquilliser and 26 per cent other prescribed drugs. There was an 11 per cent increase in the number of presentations involving street drugs, from 420 in 2013 to 465 in 2014 (following annual decreases from in 2010 to 2013). The 2014 level was similar to the level recorded in 2008 – 461.
The next steps, or referral outcomes, for the deliberate overdose cases were 51 per cent discharged home; 28 per cent admitted to an acute general hospital; 6 per cent admitted to psychiatric in-patient care; a small proportion (1%) refused admission to hospital; and 14 per cent discharged themselves before receiving referral advice.
The report provided information on what was being or could be done to reduce the number of self-harm cases. Particularly encouraging were the facts that over 30 self-harm specialist nurses had taken up positions in various hospitals in 2014 and that increased numbers of patients were receiving mental health assessments.
While the total number of presentations involving drug overdose rose, there was a significant reduction in overdoses involving minor tranquillisers. The report related this to proactive monitoring of prescribing patterns in primary care services since 2012. The authors recommended that reducing access to minor tranquillisers should be an on-going priority.
The authors reported that, as in previous years, alcohol continued to be one of the factors associated with the higher rate of self-harm presentations on Sundays, Mondays and public holidays, and in the hours around midnight. These findings underlined the need for on-going efforts to:
- enhance health service capacity at specific times and increase awareness of the negative effects of alcohol misuse and abuse such as increased depressive feelings and reduced self-control;
- intensify national strategies to increase awareness of the risks involved in the use and misuse of alcohol, starting at pre-adolescent age, and intensify national strategies to reduce access to alcohol and drugs;
- educate self-harm patients and their families about the importance of reduced use of and access to alcohol; and
- arrange active consultation and collaboration between the mental health services and addiction treatment services in the best interest of patients who present with dual diagnosis (psychiatric disorder and alcohol/drug abuse).
The authors reported that there was variation in the next care recommended to deliberate self-harm patients, and in the proportion of patients who left hospital before receiving a recommendation. While overall, nearly three quarters of all patients were discharged with a referral, variations were seen in referral pathways across HSE hospital groups. The authors recommended that the national guidelines for the assessment and management of patients presenting to Irish emergency departments following self-harm be implemented nationally as a matter of priority. 2
The report highlighted the on-going work by the National Suicide Research Foundation to link data on deliberate self-harm with suicide mortality data. This linking has shown that individuals who self-harm are over 42 times more likely to die by suicide than the general population. Further linkage is recommended in order to enhance insight into predictors of suicide risk.
1 Griffin E, Arensman E, Dillon CB, Corcoran P, Williamson E and Perry IJ (2015) National self-harm registry Ireland annual report 2014. Cork: National Suicide Research Foundation. https://www.drugsandalcohol.ie/24654/
2 Cassidy E, Arensman E, Keeley HS and Reidy J ((2012) Saving lives and reducing harmful outcomes: care systems for self-harm and suicidal behaviour. Dublin: HSE, and Cork: National Suicide Research Foundation. https://www.hse.ie/eng/about/Who/clinical/natclinprog/mentalhealthprogramme/selfharm/selfharm.pdf
F Concepts in psychology > Behaviour > Self-destructive behaviour / self-harm > Suicidal behaviour / suicide
G Health and disease > Substance use disorder (addiction) > Drug use disorder > Drug intoxication > Poisoning (overdose)
VA Geographic area > Europe > Ireland
Repository Staff Only: item control page