Walsh, Simone and Long, Jean
(2010)
Solvent and volatile inhalant use in Ireland.
Drugnet Ireland,
Issue 32, Winter 2009,
pp. 14-16.
Under the Irish Child Care Act 1991 it is an offence to sell, offer or make available solvents to a person aged 17 or under if there is reasonable cause to believe that he/she is likely to inhale them.
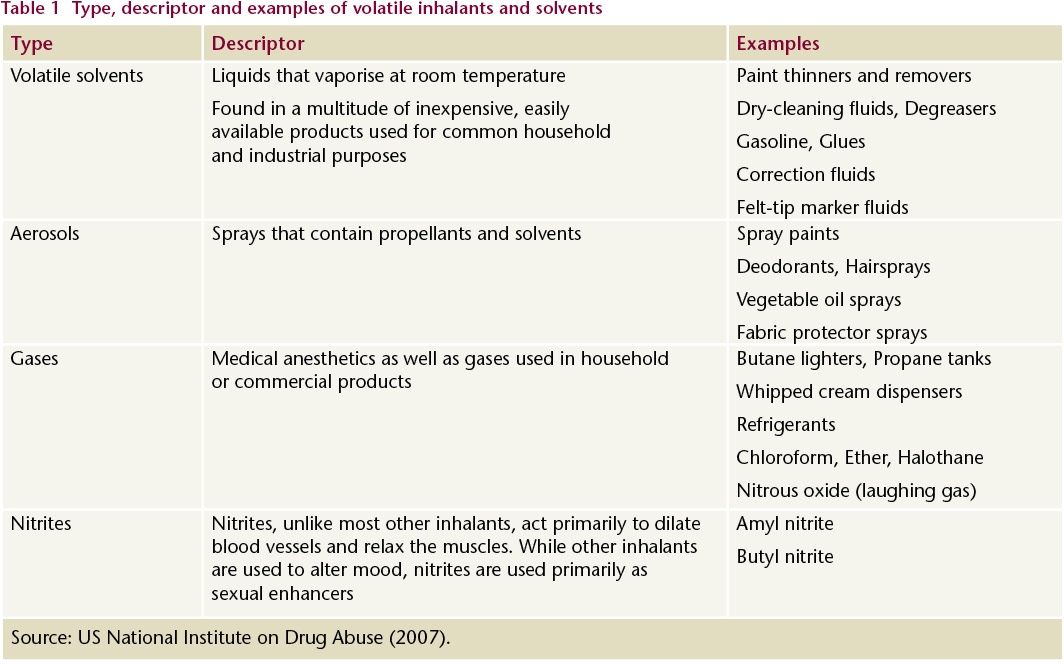
Solvents or volatile inhalants are a diverse group of substances whose chemical vapors can be inhaled to produce psychoactive or mind-altering effects.1 These substances vaporise at room temperature. A variety of products common in the home, school and workplace contain volatile substances that can be inhaled (Table 1); however, people do not typically think of these products as drugs because they were never intended to induce intoxicating effects. Yet, young children and adolescents can easily obtain these toxic substances and are among those most likely to abuse them.
NACD general population survey – volatile inhalant use
According to the 2006/7 survey,2 the proportion of the adult population who reported using a solvent or volatile inhalant in their lifetime was 1.9%, a small increase on the 2002/3 figure of 1.7%. It was more common for men (2.3%) than women (1.4%) to report use of these substances. Lifetime use was highest among adults aged 15–24 years, at 4.2%.
Survey of school children – volatile inhalant use
A study completed in 2004 examined the extent of tobacco, alcohol and drug use among primary school children aged 11 to 14 years in Limerick City, Limerick County, Clare and North Tipperary (the Mid-West Region).3 Of the 1,254 respondents to the survey questionnaire, 53 (4.2%) had used glue/solvents at least ‘once or twice’ in their lives. Forty-four out of the 53 said that they had only ever done this ‘once or twice’. Thirty-three of the solvent users were male and 20 were female.
The fourth ESPAD survey4was conducted in 35 European countries during 2007 and collected information on alcohol and illicit drug use among 15–16-year-olds. Lifetime use of solvents or inhalants decreased in Ireland over three time points, from 22% in 1999 to 18% in 2003 and to 15% in 2007, but remained higher than the European average (9%). Girls were marginally more likely to have used solvents or inhalants than boys, 16% compared to 14%. Half of the users reported that they had taken these substances three or more times during their life.
Volatile inhalant use among young people in the south east of Ireland
A recent study explored practices, social dynamics and effects of solvent or volatile inhalant use and suggested methods to deter or stop use among young people.5 This inquiry was part of a much larger study on drug use. The authors interviewed 11 males and nine females (average age 13.2 years) living in the south-east of Ireland about their solvent or volatile inhalant use. The average age of first solvent use was 10.3 years; frequency of subsequent use was sporadic and opportunistic and most stopped using by the age of 13 years. Half of the solvent users also smoked cigarettes, despite the obvious danger associated with co-use. Solvent use was followed by initiation into alcohol use (average age of first use 12.5 years) and then a small number experimented with cannabis. Most used solvents outdoors with their peer group and during the summer holidays. There were some reports of solvent use during school breaks.
The type of solvent used was determined by cost, access and place of residence. Children who lived in rural areas used a limited number of products, namely, wood glue, diesel and petrol, whereas children in urban areas used a wide variety of products, including Pritt Stick, methylated spirits, hairspray, deodorant, chrome paint, butane, nitrous oxide and Vicks nasal spray. Some products were inhaled using a plastic bag, others by placing the spray nozzle in the mouth or nostril, and others by pouring the product on a damp cloth and placing it over the face. Participants reported a variety of reasons for continuing to use solvents, such as to be part of the peer group, to relieve boredom, to experience a high, to help to deal with stress or to escape from reality. They reported a variety of physical effects such as fainting, vomiting, inflamed nostrils or headache. Some reported doing things following use that they would not normally do, such as having sex, being involved in vandalism or acting on a dare. All respondents knew someone who had died as a result of solvent use. In general, they reported that teachers were uncomfortable delivering information about drug use. They suggested that shopkeepers should not sell these substances to children. They also suggested that use would be deterred if the negative effects of these substances were explained and life stories were shared. The latter suggestion is not in line with the current evidence-based practice.
NDTRS data – treated volatile inhalant users (unpublished data)
The numbers who entered treatment in the years 2003–2007 and reported solvents or volatile inhalants as their main problem substance ranged between 24 and 32, with a total of 137 for the five-year period. The vast majority (112) of these cases were entering drug treatment for the first time. Just over half (53%) were male and four-fifths were aged 17 years or under. Only 13% lived in Dublin (possibly an indication of service availability in Dublin) and 70% were still in school. The vast majority (97%) were Irish. The solvents or volatile inhalants most commonly reported as a main problem substance were solvents (reported by 78 cases), nitrites (by 16), petrol (by 12) and butane (by 7), and the most common additional problem substances were alcohol and cannabis. In the same five-year period 164 cases reported solvents or volatile inhalants as an additional problem substance, of whom 106 were treated for the first time.
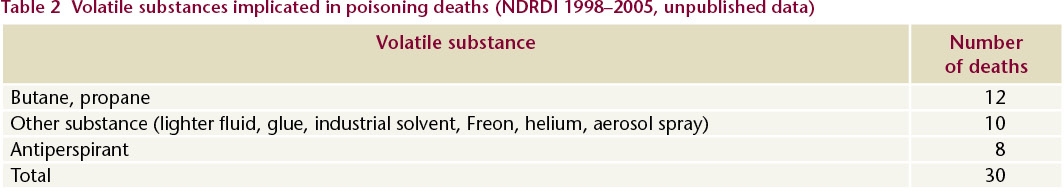
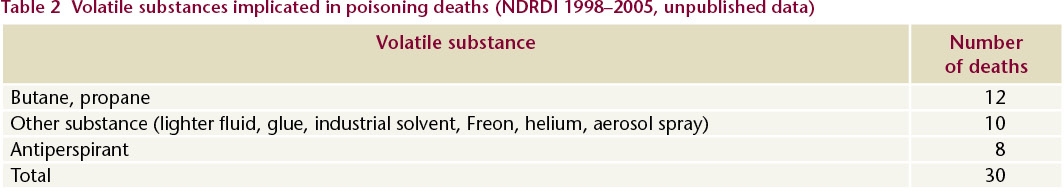
NDRDI data – deaths as a result of volatile inhalant use
The NDRDI reported 1,553 poisoning deaths in the period 1998–2005.6 Volatile inhalants and solvents were implicated in 30 of these deaths (Table 2), of which 22 were in the under-20 age group, with nine of these in the under-15 age group. Only a small number of these individuals were known to be in drug treatment at the time of their death. More than one substance was implicated in 20% of the deaths; the other substances involved were other solvents, opiates, antidepressants, benzodiazepines and alcohol. The annual death rate remained reasonably steady over the eight-year period. The male to female ratio was approximately equal (at 1.1:1). The majority (76.6%) of these individuals, including all of the under-15s, were not alone at the time of their death, and 56.6% of the deaths occurred in a private dwelling.
Conclusion
The majority of volatile inhalant or solvent users are teenage boys and girls who are still in school. Only a small number seek treatment for problematic use of these substances. Nonetheless, there are a number of fatalities each year as a result of inhaling these everyday household products.
In early 2006, the Justice Department of the Scottish Executive commissioned a review of the available evidence on volatile substance abuse among young people in Scotland.7 The topics covered in the review were the prevalence and nature of volatile substance abuse, successful prevention of such abuse and effective communication of information and messages about such abuse. The authors reported that the available evidence was limited. Their findings indicate that:
· Volatile substances should be included in drug education and given the same priority as other illicit substances. Research is necessary to determine the appropriate age at which to introduce volatile inhalant education and identify the message(s) that should be given. This is because research carried out in England found that providing education to children about the dangers of volatile inhalant use had in some cases encouraged experimentation with volatile substances.
· Parental involvement is paramount in deterring children and teenagers from drug experimentation and continued use. Again, this means that parents must be aware of the dangers of volatile substance use, and should class these substances in the same category as other illicit drugs (such as heroin, cocaine or ecstasy).
· Manufacturers of volatile inhalants and solvents must be responsible to ensure they do all that is possible to deter abuse of these substances. This includes putting warning messages on packaging about the dangers of inhalation of these substances and designing containers that deter inhalation of the product.
· Existing legislation on the selling of volatile inhalants or solvents to minors needs to be reviewed and enforced.
· Very often volatile inhalants and solvents are classed differently to other illicit substances and are therefore not given the same priority at a policy-making level. As a result, these substances are not always specifically addressed in strategies, education programs, control and treatment.
1. National Institute on Drug Abuse (2007)
InfoFacts: inhalants. Washington DC: NIDA, Department of Health and Human Services. Accessed 11 November 2009 at
http://www.drugabuse.gov/pdf2. National Advisory Committee on Drugs and Drug and Alcohol Information and Research Unit (2008) Drug use in Ireland and Northern Ireland: first results from the 2006/2007 drug prevalence survey. Bulletin 1. Dublin: NACD.
3. Houghton F, Cowley H, Meehan F and Kelleher K (2008) Drug and solvent misuse in national school children in mid-west Ireland. Irish Journal of Psychological Medicine, 35(4): 157-158.
4. Hibell B, Guttormsson U, Ahlström S, Balakireva O, Bjarnason T, Kokkevi A et al. (2009) The 2007 ESPAD report: substance use among students in 35 European countries. Stockholm: The Swedish Council for Information on Alcohol and Other Drugs (CAN) and the Pompidou Group of the Council of Europe.
5. Van Hout MC and O’Connor S (2008) Solvent use among young Irish adolescents: a growing concern for youth workers, teachers and parents? Drugs and Alcohol Today, 8(1): 27–37.
6. Lyons S, Lynn E, Walsh S and Long J (2008) Trends in drug-related deaths and deaths among drug users in Ireland, 1998 to 2005. HRB Trends Series 4. Dublin: Health Research Board.