Mongan, Deirdre (2007) Alcohol treatments: review of effectiveness. Drugnet Ireland, Issue 21, spring 2007, pp. 14-15.
| Preview | Title | Contact |
|---|---|---|
|
PDF (Drugnet Ireland, issue 21)
- Published Version
913kB |
In November 2006 the National Treatment Agency for Substance Misuse in the UK published a report reviewing the effectiveness of treatments for alcohol problems.1
Alcohol use exists along a continuum from problem-free use to very harmful and dependent use. A significant proportion of those who develop alcohol problems in the general population recover without formal treatment, but by responding to support and direction from family and friends or to self appraisal of the problem drinking. Those who seek treatment have typically experienced prolonged alcohol-related problems in health, relationships and finances and have had previous, failed, unassisted attempts at changing drinking behaviour.
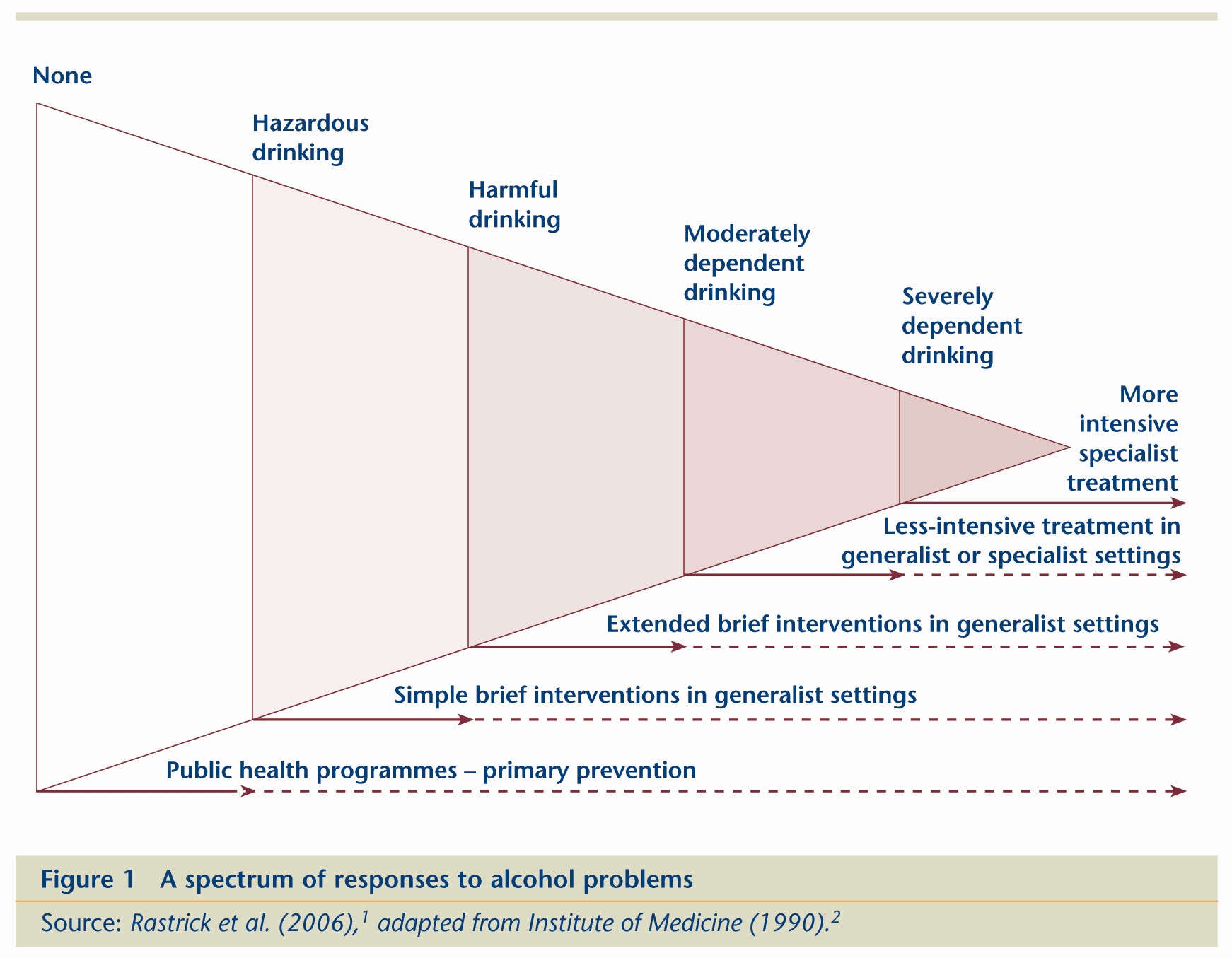
Traditionally, alcohol treatment has had a narrow focus, concentrating on ‘alcoholics’ or those with severe alcohol dependence. It is now recognised that this exclusive focus needs to be broadened to include the large group of drinkers whose problems are less severe. Early intervention, before excessive drinking has produced a level of alcohol dependence that renders treatment difficult, is associated with better outcome and cost effectiveness. Treatments for harmful and hazardous drinkers may involve providing brief treatment or information and advice in an out-patient setting, whereas treatment for problem or dependent drinkers may involve complicated detoxification in residential settings (Figure 1).
Early detection is essential to identify problem drinkers who have not sought help, and targeted rather than universal screening is recommended. Screening instruments include questionnaires, biological markers of recent alcohol consumption and clinical indicators using clinical history or signs at physical examination. The AUDIT (Alcohol Use Disorders Identification Test) questionnaire has good sensitivity and specificity for detecting hazardous and harmful drinking and has been validated for use in a wide range of settings and populations.
The types of treatment available can be categorised into three groups – psychosocial treatment, non-alcohol-focused specialist treatment and pharmacotherapies. Psychosocial treatments typically focus on helping clients both to develop better skills and to improve their environment, and those with a clear structure and well-defined interventions have positive effects on alcohol problems. Non-alcohol-focused specialist treatments include coping skills, counselling, family work and complementary therapies and have a strong evidence base. Pharmacotherapies treat alcohol problems with drugs, including detoxification medications, relapse-prevention medications and nutritional supplements.
The Mesa Grande is a type of league table based on accumulated evidence of treatment effectiveness from controlled trials and is useful as a broad indicator of which treatments are supported by research evidence. The treatments deemed most effective by this method fall mainly under the heading of ‘cognitive-behavioural therapy’, a psychosocial treatment based on social learning therapy. There is strong evidence for the effectiveness of this therapy among those with severe drinking problems. Two kinds of pharmacotherapy are also well supported by research evidence – acamprosate and naltroxone – but are best regarded as adjuncts to psychosocial treatment.
Brief interventions are given the highest rank in the Mesa Grande and are directed at hazardous and harmful drinkers who, typically, are not complaining about or seeking help for an alcohol problem. They are carried out in general community settings and are delivered by non-specialist personnel. Brief interventions, of various forms and delivered in a variety of settings, are effective in reducing alcohol consumption to low-risk levels, but most healthcare professionals have yet to incorporate screening and brief interventions for hazardous and harmful drinking into their routine practices.
Less intensive treatments are aimed at help-seekers and are usually delivered by specialist workers in alcohol treatment agencies. They are intended mainly for moderately dependent drinkers and are cheaper to deliver than conventional, more intensive treatments. These treatments often involve the participation of relatives and friends in the treatment process. Examples of such treatments include motivational interviewing, motivational enhancement therapy, brief conjoint marital therapy and condensed cognitive behavioural therapy. Motivational enhancement therapy is ranked second in the Mesa Grande.
For service users with moderate or severe alcohol dependence, alcohol-focused treatments in specialist alcohol or addiction services are most appropriate. The cognitive behavioural family of interventions is well researched and is shown to be effective for this group of service users. These treatments concentrate on the service user’s drinking and alcohol-related problems and are best deployed in community settings where the service user has the opportunity to try out newly learned behaviour in the real environment and get immediate feedback on performance. Examples include community reinforcement approach, social behaviour and network therapy, behavioural self-control training and coping and social skills training.
Pharmacotherapies are generally targeted at a narrow spectrum of symptoms or psychological problems and are usually insufficient to constitute a treatment package when given alone. Pharmacotherapies, when combined with psychosocial therapies, consistently improve addiction outcomes. Detoxification is a common procedure which may be undertaken in any treatment setting and chlordiazepoxide is the drug of choice for uncomplicated detoxification. Relapse-prevention medication includes sensitising agents which produce an unpleasant reaction when taken with alcohol, and anti-craving medications which act upon endogenous neurochemical systems to reduce alcohol cravings. An example of a sensitising agent is disulfiram, while naltrexone and acamprosate are examples of anti-craving medications.
There is no best treatment or intervention for alcohol problems. Rather, there is a range of effective treatments for different types of service user in different settings. People whose problems are more complex by virtue of severe dependence, psychological morbidity or social disorganisation are likely to need more intensive treatments. The selection of which treatment to offer therefore depends on clinician preference, client choice and availability of trained and enthusiastic therapists. Effective treatment requires a delivery system that has the following three components: organisational support to clinical services, well-trained therapists and a repertoire of specific interventions that meet service users’ needs. The stepped-care model of treatment represents a cost-effective implementation of treatment services. The basic principle of this approach is that alcohol misusers are initially offered the least intrusive and least expensive intervention that is likely to be effective.
Providing effective treatment is likely to significantly reduce the social costs relating to alcohol as well as improving individual social welfare. The variation in the course of alcohol problems over time means it is a better investment to spend fewer healthcare resources during each contact with the service user, while allowing the intervention to extend over a longer period. Although healthcare costs may increase in the short term for drinkers who have not accessed healthcare services prior to alcohol treatment, they are likely to decrease thereafter. It is claimed that for every £1 spent on treatment in the UK, £5 is saved elsewhere, making alcohol treatment highly cost effective in comparison with other healthcare interventions.
1. Raistrick D, Heather N, Godfrey C (2006) Review of the effectiveness of treatment for alcohol problems. London: National Treatment Agency for Substance Misuse.
2. Institute of Medicine (1990) Broadening the base of treatment for alcohol problems. Washington DC: National Academies Press, Figure 9.1.
B Substances > Opioids (opiates) > Opioid product > Naltrexone
G Health and disease > Substance use disorder (addiction) > Alcohol use disorder
G Health and disease > Substance use disorder (addiction) > Alcohol use disorder > Alcohol withdrawal / craving
HJ Treatment or recovery method > Substance disorder treatment method
HJ Treatment or recovery method > Treatment outcome
VA Geographic area > International
Repository Staff Only: item control page