Lyons, Suzi (2015) Predicting retention in MMT in Ireland. Drugnet Ireland, Issue 55, Autumn 2015, pp. 20-21.
| Preview | Title | Contact |
|---|---|---|
|
PDF (Drugnet Ireland 55)
3MB |
A cross-sectional study of clients attending a large methadone clinic in Dublin was conducted in March 2012, with the aim of identifying the factors associated with relapse from methadone maintenance treatment (MMT) and the reasons for the relapse.1
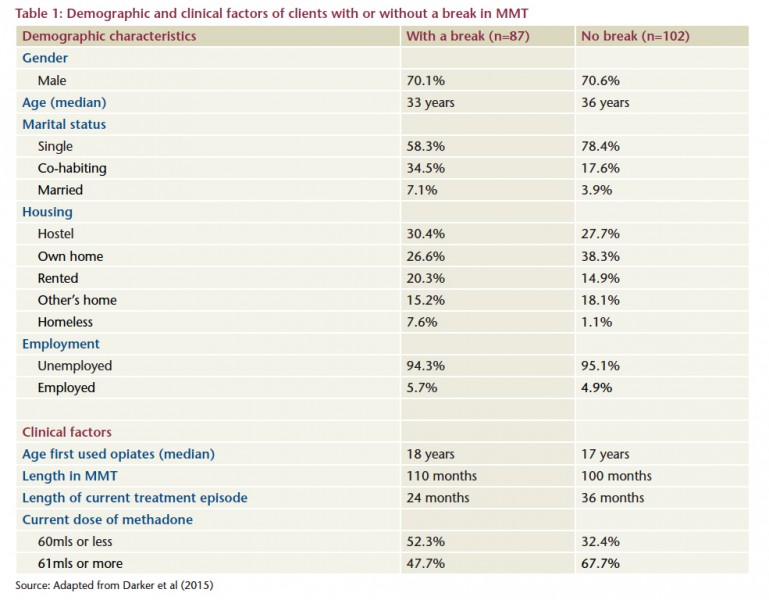
Almost two thirds (189, 63%) of the total 300 clients attending the clinic in March 2012 participated in the study. A researcher administered a questionnaire collecting data on demographic characteristics and clinical factors and asked a series of open-ended questions regarding reasons for breaking treatment. Participants were categorised into two groups: those who had had a break in their MMT (n=87, 46%) and those with no break in their MMT (n=102, 54%).
The demographic profile of both groups was relatively similar (Table 1). The majority were male and single, and there was a very high level of unemployment in both groups. A higher proportion of those with a break in MMT were homeless (7.6% versus 1.1%), and co-habiting was more common among those with a break in MMT (34.5% versus 17.6%). The median age of those with a break was 33 years, slightly younger than those with no break (36 years).
Clinical factors were also similar in both groups (Table 1), although just over half (52.3%) of those with a break in MMT were taking a methadone dose of 60mls or less compared with only 32.4% of those with no break.
Of those who ever had a break in MMT, most only reported one break (83.9%, 73). The length of break varied from less than one month to 18 months but the median duration was two months. Females were more likely to have had shorter breaks compared to males but no other factors were found to be significant in relation to duration of MMT.
Statistical analysis showed that age was the only demographic factor significantly associated with not having a break: older clients were less likely to have a break in MMT. Three clinical factors were significantly associated with not having a break: current methadone dose higher than 60 mls, longer time in treatment, and less than one year in current treatment episode. In addition, although the numbers were small, nine out of the ten clients with a prescription for anti-psychotic medicine did not report a break in treatment.
The most common reasons for breaks in MMT reported by the study participants were:
- 21.8% – relapse to drug use
- 13.7% – ‘fed up with methadone’ and wanting to detox off
- 11.4% – imprisonment or problems with the police
- 10.3% – difficulty with travelling to the clinic or clinic times
- 8.0% – being ‘clean’
- 6.8% – being out of the country
- 6.8% – emotional events, e.g. family bereavements
- 3.4% – not wanting to take methadone while pregnant
- 3.4% – illness.
Reasons given for regular attendance were:
- 37.5% – wanting to get or stay ‘clean’
- 16.1% – wanting to avoid sickness
- 13.9% – methadone dependence
- 10.2% – level of services provided by clinic
- 5.1% – withdrawal symptoms
- 5.1% – support from family members
- 4.4% – only having to attend a few times a week.
The findings of this study in relation to older age and higher methadone dose being predictors of retention in MMT correspond with the findings of other national and international research studies. The authors state that the finding in relation to anti-psychotics was unexpected, although the numbers involved were very small. They refer to published literature suggesting that Olanzapine, an antipsychotic drug, has been found to increase retention among clients with schizophrenia and that very occasionally methadone has been used to treat psychotic symptoms. The most common reason for break in treatment reported in other studies has also been relapse to drug use.
While the study confirms that higher methadone doses may improve retention in treatment, the authors recommend that this should be balanced against the known side-effects of increasing the dosage, e.g. constipation, hypotension, drowsiness and increased dependence. The second recommendation is in relation to prescribing anti-psychotics to clients with psychotic disorders in order to improve retention. The authors also recommend that further research be carried out to explore the impact of schizophrenia on MMT and that more in-depth research be carried out on the reasons for breaks in treatment in those groups known to be at higher risk.
- Darker C, Ho J, Kelly G, Whiston, L and Barry J (2015) Demographic and clinical factors predicting retention in methadone maintenance: results from an Irish cohort. Irish Journal of Medical Science, Early online. https://www.drugsandalcohol.ie/24022/
HJ Treatment or recovery method > Substance disorder treatment method
HJ Treatment or recovery method > Substance disorder treatment method > Substance replacement method (substitution) > Opioid agonist treatment (methadone maintenance / buprenorphine)
HJ Treatment or recovery method > Treatment outcome
VA Geographic area > Europe > Ireland
Repository Staff Only: item control page