Lyons, Suzi (2015) Urban overdose hotspots in Dublin. Drugnet Ireland, Issue 53, Spring 2015, pp. 11-12.
| Preview | Title | Contact |
|---|---|---|
|
PDF (Drugnet Ireland 53)
2MB |
Globally, opioids are one of the main causes of death among problem drug users. In countries with a high prevalence of heroin use, including Ireland, opiates are implicated in the majority of overdoses. Acute opioid overdoses impose a considerable burden on frontline health services such as ambulances and emergency departments. While the impact of environmental factors (e.g. deprivation, physical characteristics of area, allocation of health services) on the incidence of overdose has not been widely studied, historical data show that overdoses and associated fatalities are more common in areas where there is increased drug use, drug dealing and other drug-related activities, and addiction services have been set up in these areas.
A recent study looked at opioid overdoses in Dublin in order to understand more fully the risk factors involved, to help reduce the associated mortality and morbidity and to improve the response to such incidents.1 The study had two aims: to establish a baseline incidence of all new overdoses that Dublin ambulances attend, and to look at the relationship between geographical location of overdoses, deprivation and location of methadone clinics.
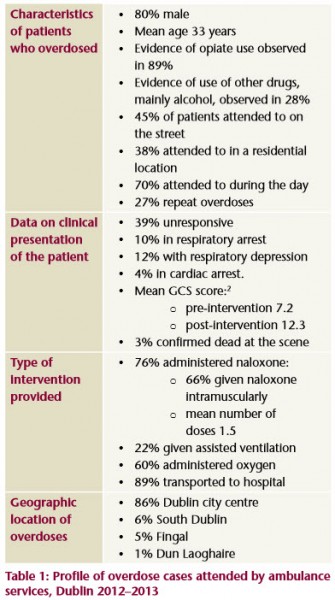
There are two ambulance services in Dublin: the Dublin Fire Brigade (DFB), and the National Ambulance Service (NAS) operated by the Health Service Executive (HSE). Ambulance staff enter data on each individual that they attend on a patient care report (PCR). The PCR is a paper-based record of the pre-hospital care given by ambulance staff/first responders. All PCRs for a 12-month period in 2012–2013 were reviewed prospectively to identify opioid overdoses. All relevant data were extracted: clinical presentation; clinical care provided; administration of naloxone; response to naloxone; whether the patient was taken to hospital; and death, if confirmed by ambulance staff on scene. Follow-up data on patients who were taken to emergency departments were not collected for this study.
The locations of overdoses were categorised as ‘street’, ‘residential’ (house/hotel) or ‘service’ (homeless shelter, treatment centre, hospital, shop, pub, Garda station). DFB personnel assigned geographic co-ordinates for the location of every overdose attended. These data were not available for attendances by the NAS.
Over the study period, ambulances attended 469 opioid overdoses. This gives an overdose incidence of 4.9 cases per 1,000 cases per year.
The relationship between overdose and deprivation was examined using the Pobal-Haase-Pratschke Deprivation Index and pre-existing Small Area (SA) boundaries.3 The Deprivation Index is a composite score ‘measuring the relative affluence or disadvantage of a particular geographic area’. The score ranges from -40 (most disadvantaged) to +40 (most affluent). Each overdose was mapped to its corresponding SA. There were some statistically significant differences found between:
- the number of overdoses and level of area affluence, with a greater number of overdoses occurring in less affluent areas, and
- the locations where overdoses occurred, with overdoses occurring in residential locations having a lower deprivation score than overdoses occurring in street locations.
The study also looked at the location of methadone clinics in relation to overdoses. This showed that most overdoses occurred within a 1,000-metre radius of certain methadone clinics.
The authors identified some limitations to the study. PCR forms were not always reliable (they were hand-written under stressful circumstances and often involved difficult decisions) and data could not be validated. Geo-data were not available for NAS PCRs.
The results of the study highlight several issues which can help inform decisions about preventing overdose deaths. Dublin ambulance services attended an opioid overdose almost daily; the majority occurred in Dublin city centre, on the street, during the day and near certain methadone clinics; street overdoses were more likely to occur in the city centre and on the quays, while residential overdoses were more likely to occur in the suburbs. Clinical findings showed patients had low mean GCS scores pre-intervention, meaning that many patients were unconscious. However, the mean GCS scores post-intervention showed improvement, indicating the effectiveness of the intervention given by the ambulance staff. However, the results also showed that the GCS scores of 25% of patients did not improve after administration of naloxone.
Despite international research indicating that overdose prevention and naloxone distribution programmes can help to reduce overdose deaths, not many countries provide such programmes.4 The authors stated that the results point to the need for such a programme, based in the community, in Ireland.
-
limas J, O'Reilly M, Egan M, Tobin H and Bury G (2014) Urban overdose hotspots: a 12-month prospective study in Dublin ambulance services. The American Journal of Emergency Medicine, accepted manuscript (in press). https://www.drugsandalcohol.ie/22440/
-
Small area (SA) boundaries are subdivisions of pre-existing electoral districts created by the Central Statistics Office. www.cso.ie/census
-
Lyons S (2014) Preventing opiate-related deaths in Ireland: the naloxone demonstration project Drugnet Ireland (49): 13. https://www.drugsandalcohol.ie/21677/
Repository Staff Only: item control page