Long, Jean and Lyons, Suzi
(2010)
Problem opiate use in Ireland.
Drugnet Ireland,
Issue 32, Winter 2009,
pp. 11-14.
An opiate is a drug containing opium or any of its derivatives which acts as a sedative and narcotic. Examples include heroin, methadone, morphine, codeine, hydrocodone, oxycodone, fentanyl and tramadol. Heroin is synthesised from morphine, a naturally occurring substance extracted from the seed pod of the Asian opium poppy plant.1 Heroin is available in three forms – a white powder, a brown powder or a black sticky substance, known as ‘black tar heroin’.
Data sources
In a repeat of a similar prevalence study in 2001–2001,2 Dr Alan Kelly and colleagues estimated the prevalence of problem opiate users in Ireland in 2006 using a three-source capture-recapture method.3 The three data sources used were the Central Treatment List (of clients on methadone), the Hospital In-Patient Enquiry scheme and the Garda PULSE data. This article highlights some of the study findings and presents data from the National Drug Treatment Reporting System (NDTRS),4 the National Drug-Related Deaths Index (NDRDI)5 and the Central Statistics Office (CSO).6
Estimation of the numbers of adult problem opiate users
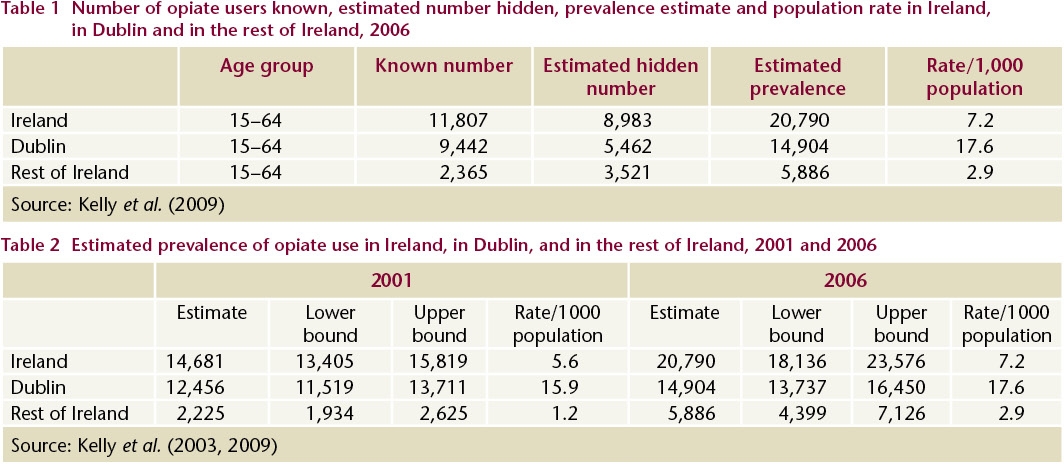
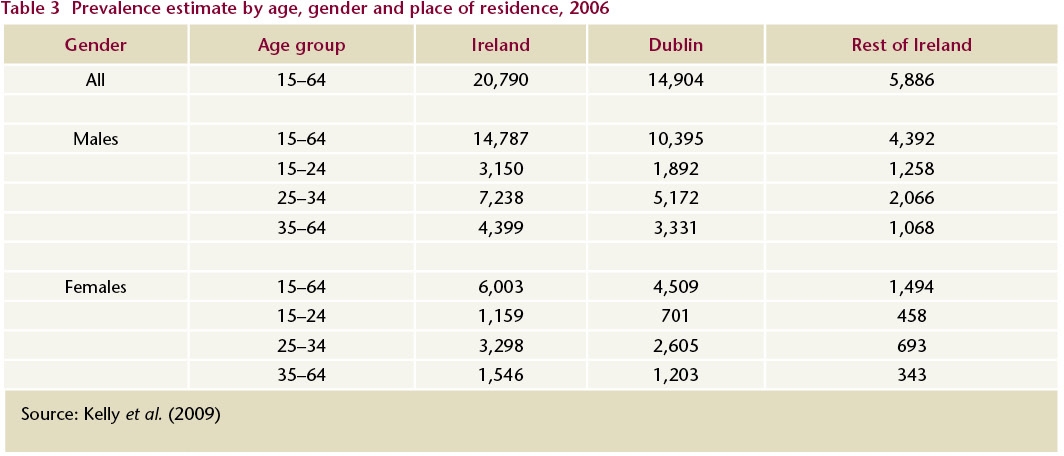
Data from the three sources indicated that there were 11,807 opiate users aged 15–64 years known to services in Ireland in 2006, and an estimated 8,983 users not known to the services (hidden population) (Table 1). The national prevalence estimate of opiate users in 2006 was between 18,136 and 23,576; the point estimate was 20,790 (Table 2). This estimate is likely to be inflated (see footnote).7 Twenty-eight per cent (5,886) of the estimated number lived outside Dublin and 72% (14,904) lived in Dublin. The respective rates per 1,000 of the 15–64-year-old population in Dublin and in the rest of Ireland are 17.6 and 2.9.
The point estimate increased by 42%, from 14,681 in 2001 to 20,790 in 2006. The point estimate for Dublin increased by 20%, while the point estimate for the rest of Ireland increased by 165% – albeit from a low estimate in 2001. The rate of opiate use per 1,000 of the 15–64-year-old population living outside Dublin increased from 1.2 in 2001 to 2.9 in 2006.
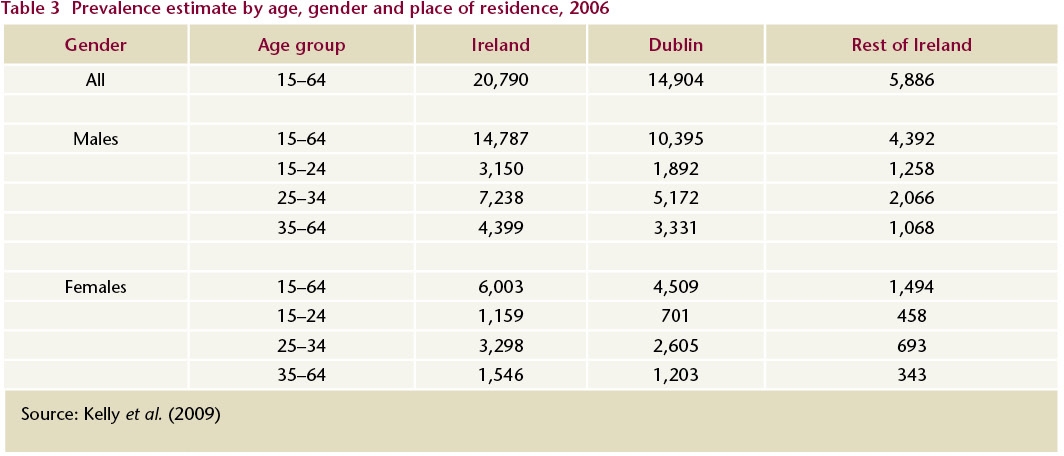
Table 3 shows the 2006 estimate by age, gender and place of residence. Seventy-one per cent were male. One in five (21%) was between 15 and 24 years old and half (51%) were between 25 and 34 years old. In Dublin, the rate of opiate use per 1,000 of the 15–24-year-old female population decreased by 62%, from 18.7 in 2001 to 7.2 in 2006, which indicates that the number of younger women commencing opiate use has decreased. A smaller but still notable decrease in the rate of opiate use in Dublin was seen among males aged 15–24 years.
In an unpublished study, Kelly and colleagues report that retaining opiate users in treatment reduces their likelihood of being in contact with the gardaí (Dr A Kelly, personal communication, 2009). For example, only 12% of males aged 25–34 years who were known to the gardaí in 2001 and were attending treatment services between 2001 and 2006 were reported to be committing crime in 2006. This is in line with findings from the ROSIE study8 and indicates that methadone treatment reduces the incidence of crime.
NDTRS data – treated opiate users
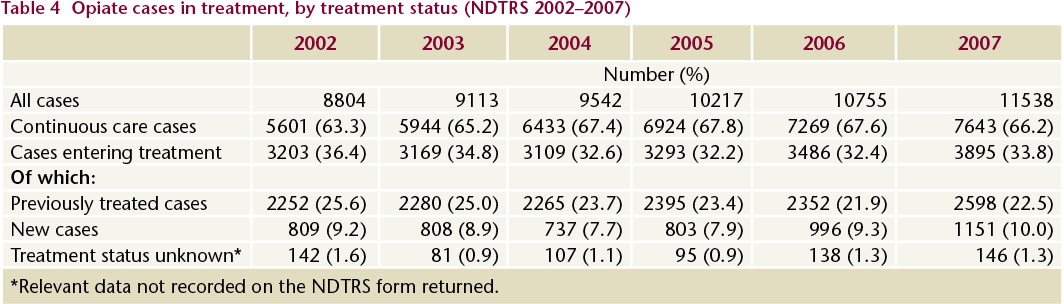
In 2007, 11,538 cases were treated for problem opiate use.4 This is a 31% increase (2,734 cases) since 2002 and an increase of just over 7% (783 cases) since 2006 (Table 4).
- Two-thirds (7,643) of problem opiate users were continuing in care, that is, they were already in methadone treatment on 31 December 2006 and continued to receive that treatment after 1 January 2007.
- Just over one-fifth (2,598) had received treatment before and re-entered treatment in 2007. This reflects the fact that problem opiate use is a recurring problem and requires repeated treatment over time.
- Ten per cent (1,151) were new cases presenting for treatment for the first time.
- A small number of cases (146, 1.3%) were not clearly identified as either new or return cases.
Of the 3,575 previously treated and new cases who entered treatment in 2007 and who reported opiates as their main problem substance, more than half used it daily, 10% used it on two to six days per week and 6% used it once a week or less. One-quarter had not used it in the month prior to treatment; this reflects the transfer of stable clients to other types of treatment centres, such as general practice and medication-free residential services.
Between 2002 and 2007, 5,304 cases entered treatment for the first time. The rate of new cases aged 15–64 increased from 28 per 100,000 in 2002 to 35 in 2007. The overall number of opiate cases was high in Dublin; however, the number of new cases was lower in 2007 than in 2002. Over the same period there was a significant increase in new cases elsewhere in the country, with a steady increase in the midland, south eastern and north eastern counties. The number of new cases is an indirect indicator of recent trends in problem substance use.
There was a 54% (2,680) increase in the number of methadone treatment places between 2001 and 2007. This reflects one of the benefits of the proactive approach of the National Drugs Strategy. It is important to note that methadone substitution is a long-term treatment that can take a number of years to show results.
Of the 3,575 cases who entered treatment and reported opiates as their main problem substance in 2007, 52% smoked it, 40% injected it and 5% consumed it orally. From 2003 to 2007, decreasing proportions of cases reported injecting as their primary route of administration, while correspondingly increasing proportions reported smoking as their primary route.
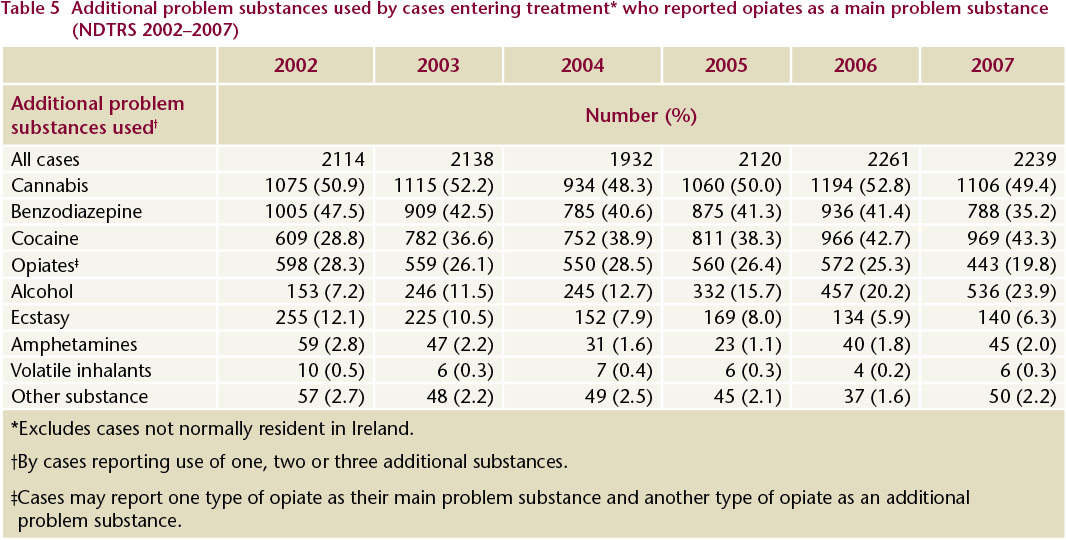
The proportion of cases treated for opiates as a main problem substance who reported use of more than one substance decreased from 69% in 2002 to 63% in 2007. The decrease in polydrug use was observed among both new and previously treated opiate cases, but was more marked among the new cases. The reason for the decrease is not clear; it may be the result of an increase in the number of newer opiate users who have yet to develop chronic polydrug-using practices, or of improved history-taking practices by service providers. Polydrug use is one of the factors that can impede successful treatment for problem opiate use. Specific interventions, such as detoxification from other drugs and contingency management, are required to address this problem.
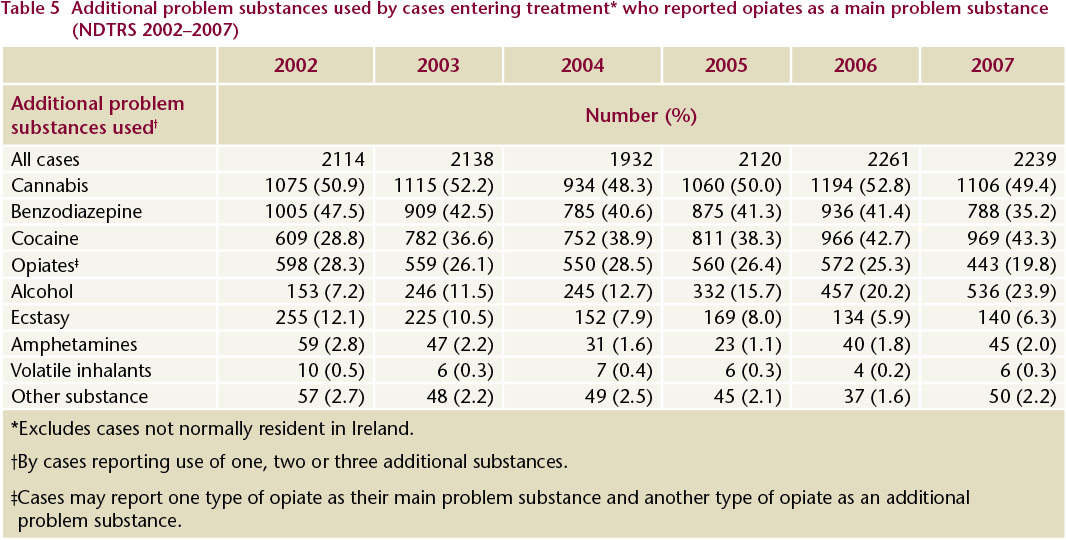
Table 5 shows the additional problem substances used by cases entering treatment who reported opiates as their main problem substance. Between 2002 and 2007, cannabis, benzodiazepine and cocaine were the most common additional problem substances reported. Cannabis was top of this list in each of the six years. Benzodiazepine was the second most common additional substance between 2002 and 2005, but was replaced by cocaine in 2006 and 2007. The number reporting cocaine as an additional problem substance increased by 59% over the period. The number reporting alcohol as an additional problem substance increased by 250% over the period.
NDRDI data – deaths among opiate users
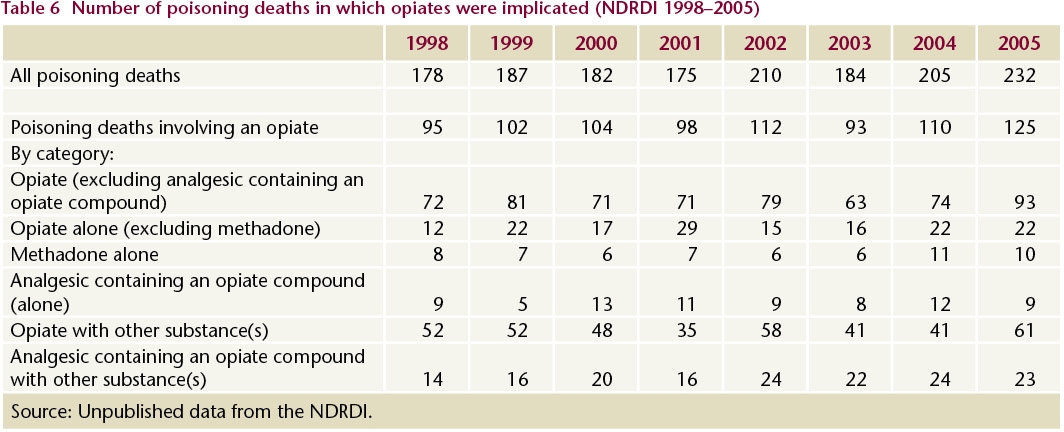
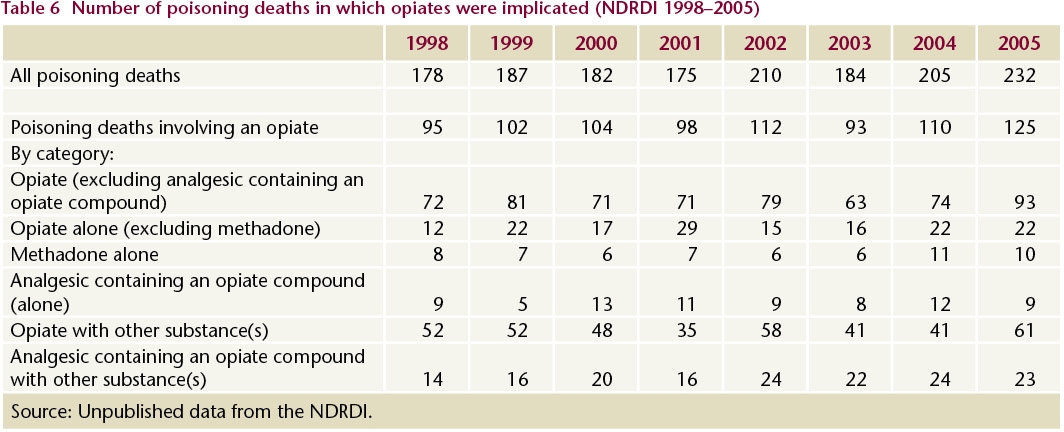
The NDRDI reported that there were 1,553 deaths as a result of poisoning between 1998 and 2005.5 In over half (839, 54.0%) of these deaths, heroin, methadone or other opiates were implicated (either alone or in conjunction with other substances) (Table 6). Over one-third (292, 34.8%) of the opiate-related deaths were attributable to a single opiate. Of all the poisoning cases involving an opiate, 634 (75.6%) were male and 657 (78.3%) were aged between 20 and 44 years; of those for whom employment status was known, 445 (62.4%) were unemployed.
CSO data – drug seizures
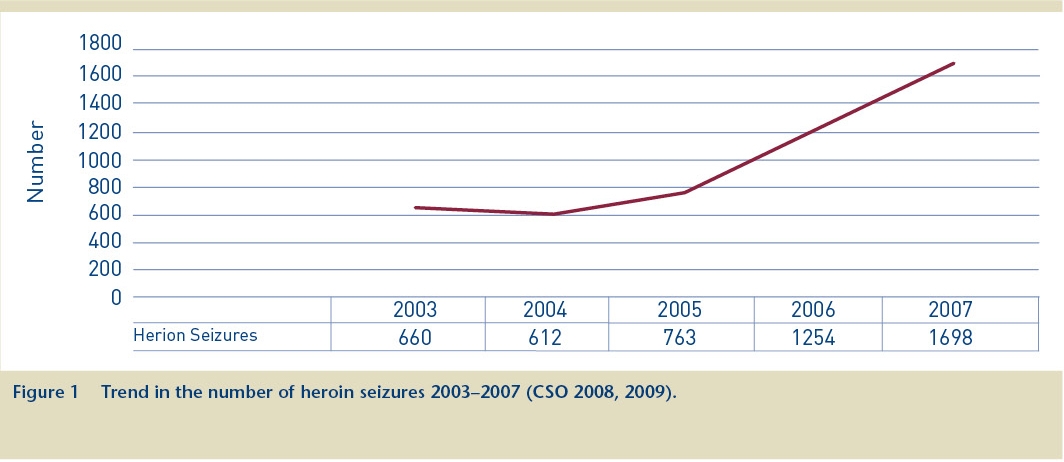
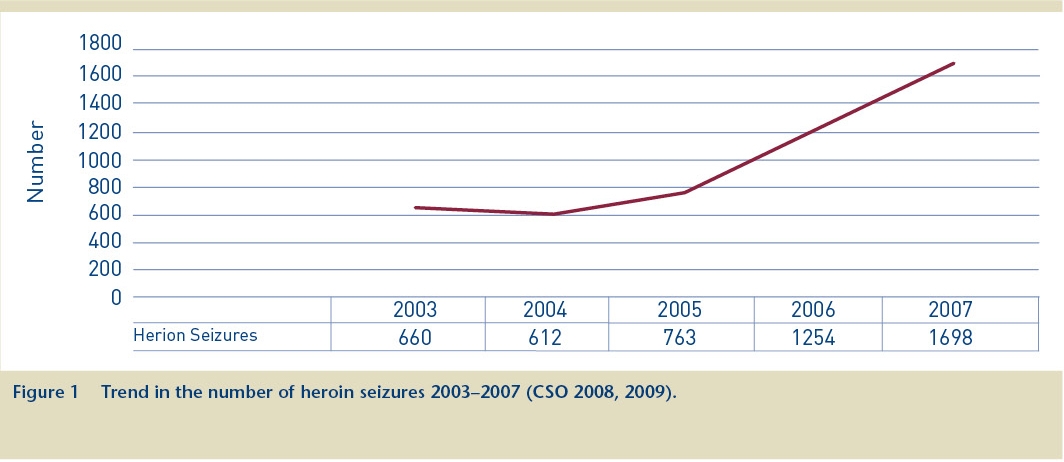
Figure 1 presents the number of heroin seizures in the years 2003–2007, showing a steady rise since 2004.
Conclusion
The data from a range of sources indicate an increase in opiate availability, and a parallel increase in use and in treatment demand. The data also point to the serious consequences of opiate use, most notably the considerable number of deaths each year in which an opiate is involved.
2. Kelly A, Carvalho M and Teljeur C (2003) Prevalence of opiate use in Ireland 2000–2001: a 3-source capture-recapture study. Dublin: Stationery Office.
3. Kelly A, Carvalho M and Teljeur C (2009) Prevalence of opiate use in Ireland 2006: a 3-source capture- recapture study. Dublin: National Advisory Committee on Drugs.
4. Carew AM, Bellerose D, Lyons S and Long J (2009) Trends in treated problem opiate use in Ireland, 2002 to 2007. HRB Trends Series 7. Dublin: HRB.
5. Lyons S, Lynn E, Walsh S and Long J (2008) Trends in drug-related deaths and deaths among drug users in Ireland, 1998 to 2005. HRB Trends Series 4. Dublin: HRB.
6. Central Statistics Office (2009) Garda recorded crime statistics 2003–2007. Dublin: Stationery Office.
7. These estimated figures are likely to be inflated because the population was not closed, that is, it continued to recruit significant numbers of people into treatment (in Dublin and outside Dublin) and police custody (outside Dublin) in 2006. In addition, the overlap between the three population sources was small. These two factors are known to inflate estimates obtained by the capture-recapture method.
8. Cox G, Comiskey C and Kelly P (2007) ROSIE Findings 4: summary of 1-year outcomes: methadone modality. Dublin: National Advisory Committee on Drugs.