Long, Jean
(2009)
Morbidity among opiate users in methadone treatment.
Drugnet Ireland,
Issue 31, Autumn 2009,
pp. 15-16.
Cullen and colleagues completed a study of problem opiate users attending general practice for methadone treatment to estimate the prevalence of chronic illness and examine patterns of health service utilisation among this group compared with matched controls.1 The cases and controls were matched for practice, age, gender and general medical service (GMS) status. Data were collected on a sample of 114 patients attending three general practices: 57 cases attending for methadone treatment (19 per practice) and 57 controls attending for primary care (19 per practice).
Illness among methadone cases
The average age of cases was 37.2 years, 42 (74%) were male, 41 (72%) had GMS cover, all were Irish nationals and 56 (98%) lived in stable accommodation. Considerable lifetime contact with the practice was observed: 16 patients (28%) had been attending the practice for less than five years, 21 (37%) for between five and 10 years, and 20 (35%) for more than 10 years. There were three reasons for initial contact with the general practice: registration for general medical care (20 patients), treatment of illicit drug use (20 patients), and referral by specialist addiction treatment services for methadone treatment (17 patients). All patients had been prescribed methadone by specialist addiction services prior to attending the general practice for methadone treatment, and 14 (25%) had been referred back to specialist addiction services since commencing methadone treatment at the practice (six in the previous year). The average dose of methadone prescribed (based on the last issued prescription) was 66 mg daily.
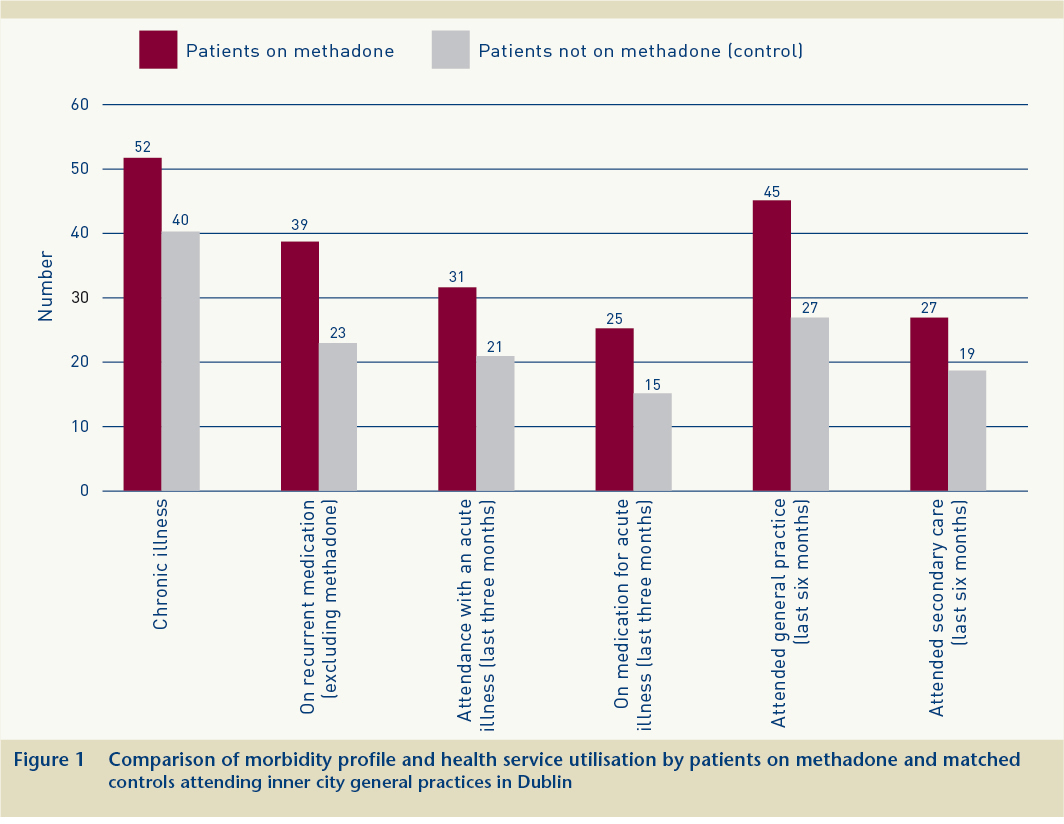
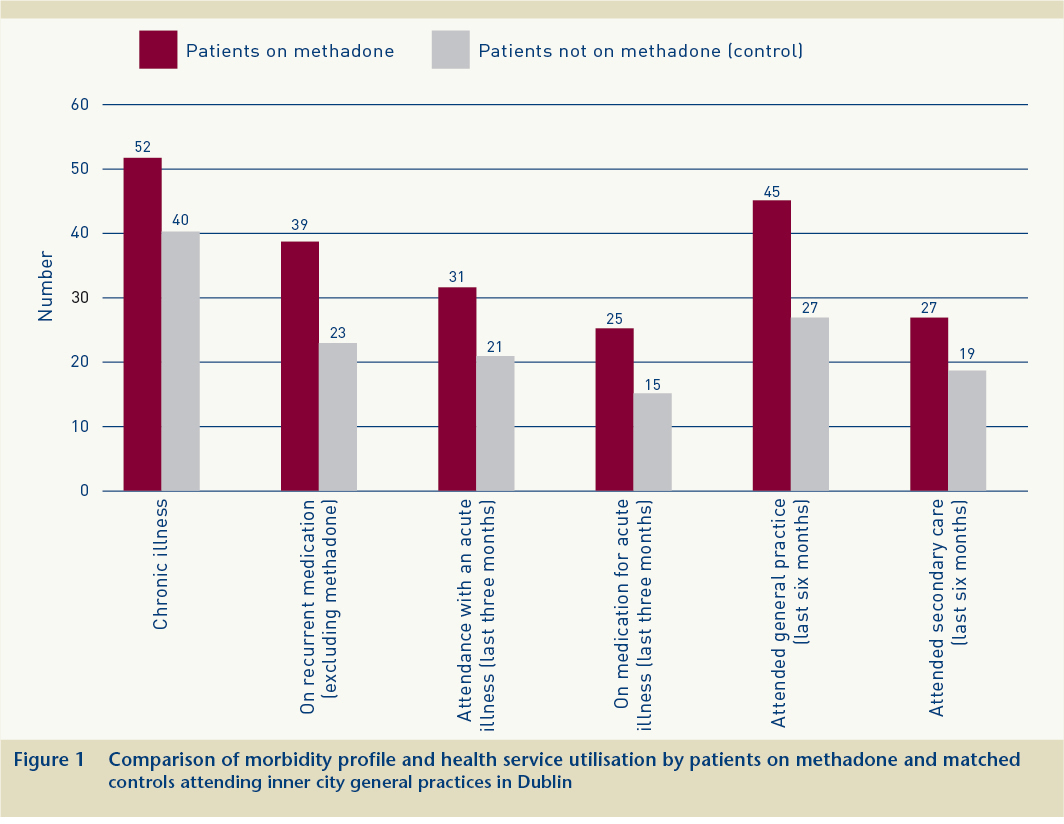
Figure 1 presents a comparison of the morbidity profile and health service utilisation characteristics of patients on methadone compared to their matched controls. Fifty-two patients (91%) had one or more chronic illnesses (in addition to opiate dependence) documented in their clinical record. Hepatitis C (38, 66%), depression (20, 35%), asthma (14, 25%), HIV/AIDS (8, 14%) and DVT/varicose veins/thrombo-phlebitis (4, 7%) were the most common chronic illnesses recorded. Thirty-nine patients (68%) were on regular prescribed medication in addition to methadone. Thirty-one patients (54%) had had at least one acute condition during the previous three months, of which the most common were: upper respiratory tract infection (10, 18%), insomnia, anxiety or depression (4, 7%), abdominal pain (4, 7%), urinary tract infection (3, 5%) and ear wax (3, 5%). Tobacco use was noted in the records of 39 patients, of whom 37 were recorded as smokers. Twenty-five patients (44%) had been prescribed at least one time-limited medication (in addition to methadone) for the treatment of an acute illness during the previous three months. In the previous six months, patients had attended their GP for issues other than their addiction care an average of four times, and27 patients (47%) had either been referred to or attended secondary care.
Comparison with matched control group
The average age of controls was 37.2 years, 42(74%) were male, 41(72%) had GMS cover, all were Irish nationals and 38 (67%) lived in stable accommodation. Morbidity and health service utilisation rates were high among this group also (Figure 1). Patients attending for methadone treatment were significantly more likely to have a chronic illness, to be prescribed recurrent medications and to attend a general practice.
1. Cullen W, O'Brien S, O'Carroll, O'Kelly FD and Bury G (2009) Chronic illness and multimorbidity among problem drug users: a comparative cross sectional pilot study in primary care. BMC Family Practice, 10(25). Accessed 14 July 2009 at www.biomedcentral.com/1471-2296/10/25